Table of Contents
Long-Bone Anatomy
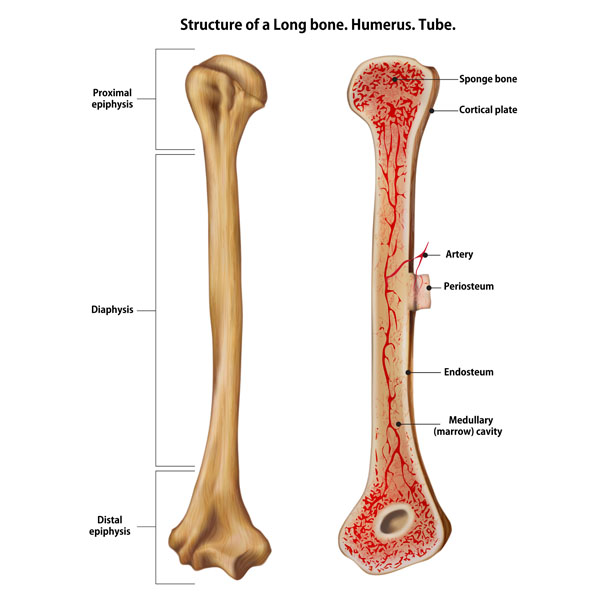
The detailed representation shows a long bone, specifically the humerus, which is the bone of the upper arm. The humerus is one of the primary bones of the arm, connecting at the shoulder to the scapula and at the elbow to the radius and ulna.
There are several key parts to a long bone:
Proximal epiphysis: This is the rounded end of the bone which is closest to the body’s midline. In the humerus, it’s part of the shoulder joint.
Diaphysis: The long, central part of the bone, also known as the shaft. It provides leverage and weight support in long bones.
Distal epiphysis: The end of the bone that is farthest from the body’s midline. In the humerus, this part forms part of the elbow joint.
The internal structure of the bone is also visible:
Sponge bone: Also known as cancellous or trabecular bone, it has a porous structure and is found at the ends of the bone. It’s designed to absorb shock and pressure, redistributing it to protect the more rigid structures of the bone.
Cortical plate: This is the outer layer of the bone, also known as the cortical or compact bone. It’s very dense and provides strength and support.
Artery: Arteries within the bone supply the bone tissue with essential nutrients and oxygen.
Periosteum: A dense, fibrous membrane that covers the outer surface of the bone except at the joints. It contains blood vessels and nerves that provide nourishment and sensation to the bone.
Endosteum: A thin vascular membrane that lines the inner surface of the bone, including the medullary cavity.
Medullary (marrow) cavity: The central cavity of bone shafts where red bone marrow and/or yellow bone marrow (fat) are stored.
This structure is representative of the anatomy found in all long bones within the human body. Each component has a specific function related to the growth, repair, and nutrition of the bone.
Microanatomy of the Bone Structure
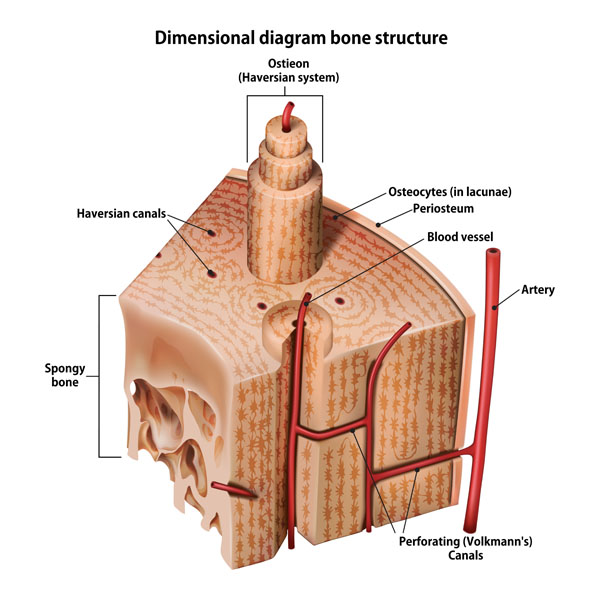
The diagram displays a portion of compact bone, highlighting the microscopic structure known as the osteon or Haversian system, and shows the relationship between different components.
Osteon (Haversian system): This is the fundamental functional unit of much of compact bone. Osteons are cylindrical structures that contain a mineral matrix and living osteocytes connected by canaliculi, which transport blood.
Haversian canals: These are small channels in the center of the osteons containing blood vessels and nerves.
Osteocytes (in lacunae): Osteocytes are mature bone cells that maintain the bone matrix and reside in lacunae, small cavities within the bone matrix.
Periosteum: This is a membrane that covers the outer surface of all bones, except at the joints of long bones. It contains osteogenic cells that are essential for bone growth and repair.
Blood vessel: The vessels within the bone that carry blood to and from the bone cells.
Artery: The large blood vessel shown here is responsible for supplying oxygenated blood to the bone.
Perforating (Volkmann’s) canals: These channels run perpendicular to the Haversian canals and connect the vascular and nerve supply of the periosteum to that of the Haversian canal.
Spongy bone: Located at the ends of bones and in the interior of vertebral bones, spongy bone is less dense than compact bone and contains spaces that are filled with bone marrow.
This detailed image underscores the bone’s rich vascular supply and its complex internal architecture, which is critical for support, protection, and the production of blood cells.
Anatomical Structures of Long Bones
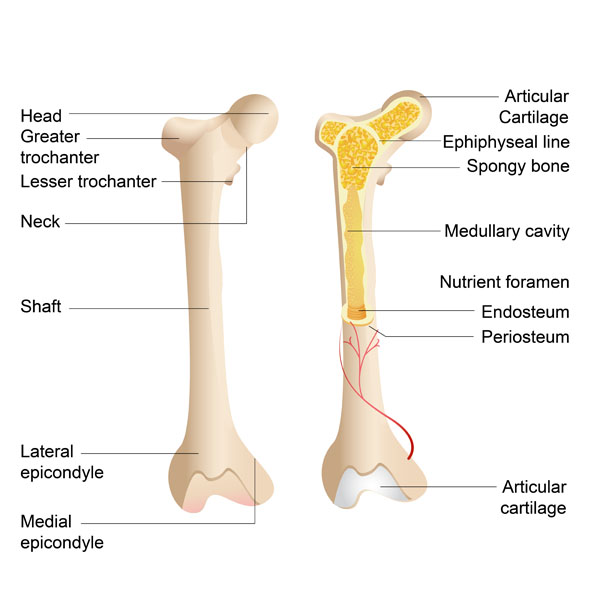
The illustration depicts two views of a long bone, showcasing both the external and internal anatomical structures.
On the left, the external features are labeled:
- Head: The rounded, proximal end of the bone, which typically articulates with another bone.
- Greater trochanter: A prominent protrusion where muscles attach, specific to the femur.
- Lesser trochanter: A smaller, posteriorly positioned protrusion on the femur for muscle attachment.
- Neck: The portion between the head and the shaft, often a narrowed area.
- Shaft: The long, cylindrical central part of the bone.
- Lateral epicondyle: A bony prominence on the lateral (outer) side of the bone, typically found at the knee or elbow.
- Medial epicondyle: A bony prominence on the medial (inner) side of the bone, also often found at the knee or elbow.
On the right, the internal structure of the bone is exposed:
- Articular Cartilage: A smooth, white tissue that covers the ends of bones where they come together to form joints.
- Epiphyseal line: The remnant of the growth plate, seen in adult bones where the epiphyseal plate once was.
- Spongy bone: The lighter, less dense bone found in the ends of long bones, containing red bone marrow.
- Medullary cavity: The central cavity of bone shafts where marrow is stored.
- Nutrient foramen: An opening in the bone that allows blood vessels to enter and nourish the bone.
- Endosteum: The lining membrane of the medullary cavity of the bone.
- Periosteum: The fibrous membrane covering the outer surface of the bone.
These structures work together to support the body, facilitate movement, protect internal organs, and store and create blood cells in the bone marrow.
Osteoporosis
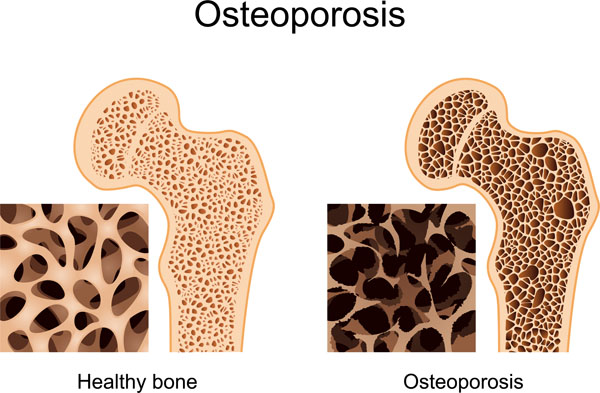
The illustration compares the internal structure of healthy bone with bone affected by osteoporosis.
On the left, the healthy bone shows a dense, tightly packed trabecular structure. This spongy bone, typically found at the end of long bones, has a honeycomb-like matrix that is designed to bear weight and support stress. The outer layer, or cortical bone, is solid and dense, adding strength and structure.
On the right, the bone with osteoporosis demonstrates a much less dense trabecular structure with larger holes and gaps. This indicates a loss of bone mass and mineral content, making the bone weaker and more prone to fractures. Osteoporosis is characterized by a decrease in the density and quality of bone, reducing its strength and resulting in bones that are fragile and at higher risk for fracture. The outer cortical bone also appears thinner, contributing to the overall weakness of the bone.
The insets show a magnified view of the trabecular bone. The healthy bone inset shows a thick, interconnected network, while the osteoporotic bone inset shows extensive bone loss, leading to a sparse and disconnected trabecular network. This comparison highlights the significant impact osteoporosis can have on bone architecture and strength.
Types of Bone Fractures
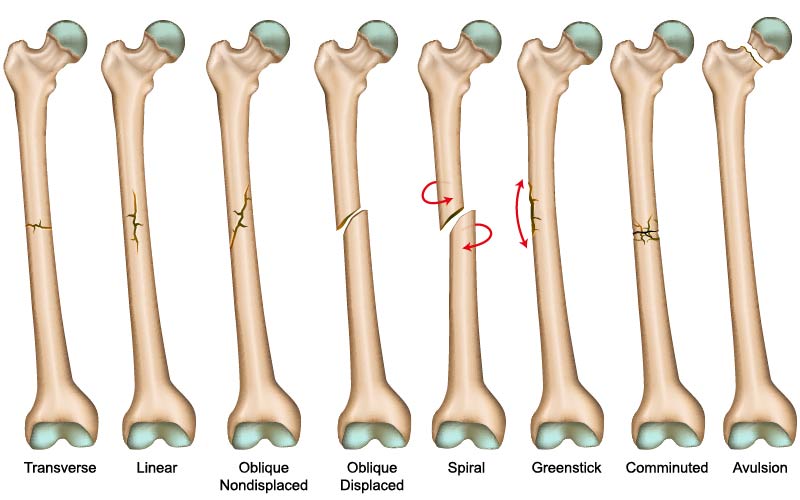
The image presents a series of diagrams depicting different types of bone fractures.
Transverse: This fracture has a horizontal fracture line across the bone shaft. It’s a straight break right across the bone.
Linear: The fracture line is parallel to the bone’s long axis. It looks like a straight line that does not traverse the entire width of the bone.
Oblique Non-displaced: This fracture has an angled line across the bone but the bone pieces remain aligned.
Oblique Displaced: Similar to the oblique non-displaced fracture, but here the bone pieces are not aligned and have shifted.
Spiral: Caused by a twisting force, the fracture line encircles the bone, resembling the stripes around a barber’s pole.
Greenstick: This is an incomplete fracture where the bone bends and cracks, instead of breaking completely into separate pieces. It’s most commonly seen in children whose bones are still flexible.
Comminuted: A fracture in which the bone is splintered into several pieces. This type often requires surgery for repair.
Avulsion: Occurs when a small chunk of bone attached to a tendon or ligament gets pulled away from the main part of the bone.
These illustrations are useful in understanding how different forces and mechanisms can cause varying patterns of bone fractures, which can affect treatment decisions and healing processes.
Bone Mass and Age
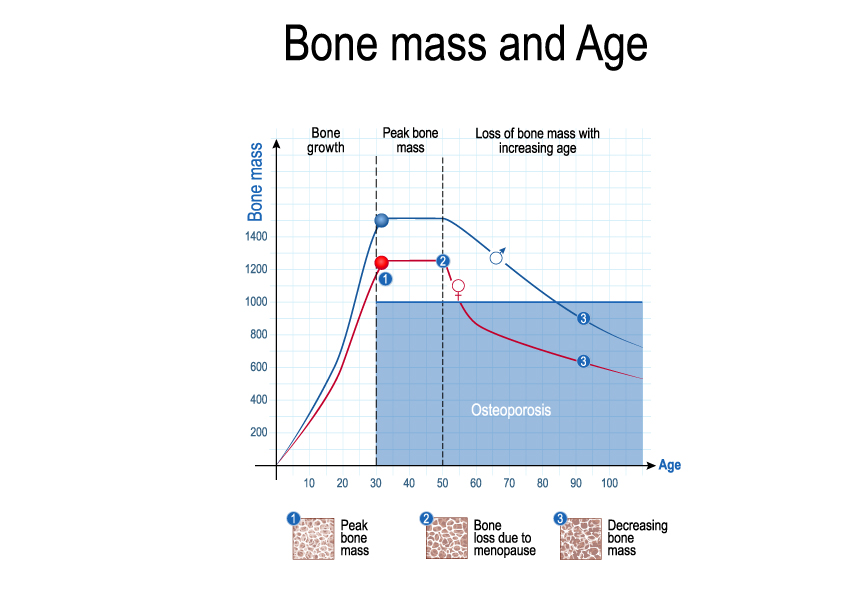
The chart depicts the relationship between bone mass and age, highlighting how bone density changes over a person’s lifetime.
The vertical axis represents bone mass, measured in arbitrary units, while the horizontal axis represents age in years. The curve demonstrates that bone mass increases during the years of growth, reaching a peak at around the age of 30, which is marked as “Peak bone mass.” This peak indicates the highest bone density that an individual will typically achieve and is a crucial factor in determining the risk of developing osteoporosis later in life.
Following the peak, the graph illustrates a gradual decline in bone mass with age. Notably, there is a marked decrease for women around the age of 50, labeled “Bone loss due to menopause.” This period coincides with significant hormonal changes that accelerate bone density loss.
The graph shows that the bone mass continues to decrease with age for both sexes, though the decline is more pronounced for women. The shaded area below the threshold line indicates the bone density level where osteoporosis becomes a concern, which increases the risk of fractures.
Overall, the graph emphasizes the importance of building strong bones through proper nutrition and physical activity during the growing years and maintaining bone health through lifestyle and possibly medical interventions in later life to mitigate the risk of osteoporosis.
Stages of Bone Healing
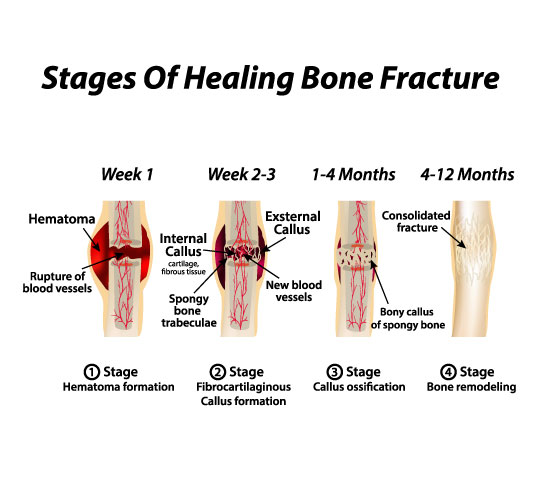
The illustration provides a concise overview of the stages of bone healing after a fracture. Bone healing is a natural process which occurs in several stages:
Hematoma Formation (Week 1): Immediately following the fracture, the disruption of the blood vessels leads to bleeding within the area, causing a hematoma, which is a localized collection of blood outside of the blood vessels. This hematoma serves as the foundation for the healing process.
Fibrocartilaginous Callus Formation (Week 2-3): During this stage, the hematoma begins to be absorbed, and fibrous tissue and cartilage (fibrocartilaginous callus) start to bridge the gap between the fracture ends. This callus is not as strong as bone and is a temporary scaffold for the upcoming bone healing stages.
Callus Ossification (1-4 Months): The callus begins to ossify or harden, as the fibrocartilaginous callus is replaced with a bony callus of spongy bone. New blood vessels develop in the area, aiding the healing process.
Bone Remodeling (4-12 Months): The final stage involves the remodeling of the spongy bone into compact bone, which may take several months to complete. The bone gradually returns to its original shape, and any excess material from the bony callus is removed. The bone’s strength and flexibility are restored through this process.
These stages reflect the complex physiological process of bone healing which involves a blend of inflammatory, cellular, and molecular mechanisms working together to restore the bone’s structure and function.
Anatomical Terms and Definitions
| Term | Definition |
|---|---|
| Avulsion Fracture | A fracture where a fragment of bone is separated from the main mass due to the pull of a ligament, tendon, or muscle. |
| Bone Density | The amount of bone mineral in bone tissue. It decreases with age, especially in women post-menopause, leading to increased risk of osteoporosis. |
| Bone Healing | The process by which bone regenerates and repairs itself after a fracture, involving several stages including hematoma formation, fibrocartilaginous callus formation, bony callus formation, and remodeling. |
| Comminuted Fracture | A fracture in which the bone is broken into several pieces. This type of fracture may require surgical intervention for proper healing. |
| Cortical Bone | The dense outer surface of bone that provides strength and structure. It surrounds the more porous cancellous bone. |
| Diaphysis | The shaft or central part of a long bone. |
| Distal Epiphysis | The end of the bone located farthest from the body's midline. |
| Greenstick Fracture | A type of fracture in which the bone bends and partially breaks, most often seen in children. |
| Hematoma | A localized collection of blood outside the blood vessels, typically in liquid form within the tissue. The first stage in bone healing after a fracture. |
| Linear Fracture | A fracture that occurs parallel to the bone's long axis. |
| Medullary Cavity | The central cavity of bone shafts where red bone marrow and/or yellow bone marrow (fat) are stored. |
| Oblique Fracture | A fracture that occurs at an angle to the bone's long axis and can be displaced or non-displaced. |
| Osteon | Also known as the Haversian system, it is the fundamental functional unit of compact bone, consisting of a central canal surrounded by concentric rings of bone matrix. |
| Osteoporosis | A condition characterized by weakened bones, making them more likely to break. Caused by a decrease in bone mass and density. |
| Periosteum | A dense, fibrous membrane covering the outer surface of all bones, except at the joints of long bones. Contains cells necessary for bone growth and repair. |
| Proximal Epiphysis | The end of the bone located closest to the body's midline. |
| Spiral Fracture | A fracture where at least one part of the bone has been twisted, often resulting from a rotating force. |
| Spongy Bone | Also known as cancellous or trabecular bone, it is found at the ends of long bones and is characterized by a porous, honeycomb-like structure. It is less dense than compact bone and contains spaces that are often filled with bone marrow. |
| Transverse Fracture | A fracture in which the bone is broken at a right angle to its long axis. |

