Table of Contents
Thoracic Aorta Anatomy
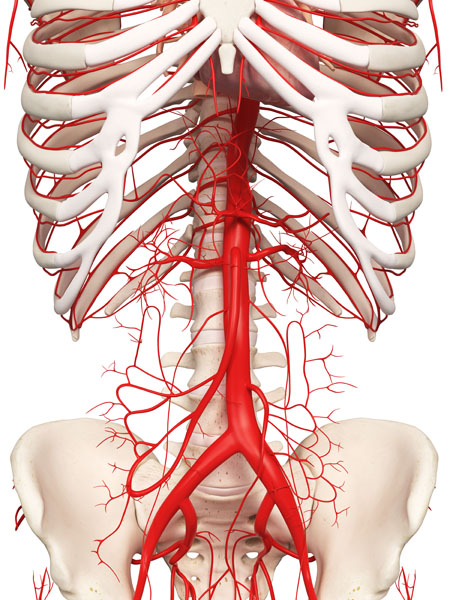
The image displays a detailed representation of the thoracic aorta and its major branches within the chest cavity. At the center, we see the thoracic aorta, which is a continuation of the aortic arch descending through the thorax. The thoracic aorta is a major artery that carries oxygen-rich blood from the heart to various parts of the body.
Emerging from the aorta are several branching vessels that supply blood to the ribs and intercostal spaces—these are the intercostal arteries. They are paired and run along the underside of each rib. Their role is to supply blood to the chest wall and the muscles between the ribs, as well as the skin and the muscles of the back.
The intricacy of the arterial network shown here highlights the body’s capacity to ensure that blood is efficiently distributed to support the metabolic needs of the thoracic structures. This illustration does not include the veins, capillaries, or other anatomical structures for clarity, focusing instead on the arterial system of the thoracic region.
Elastic Artery Anatomy
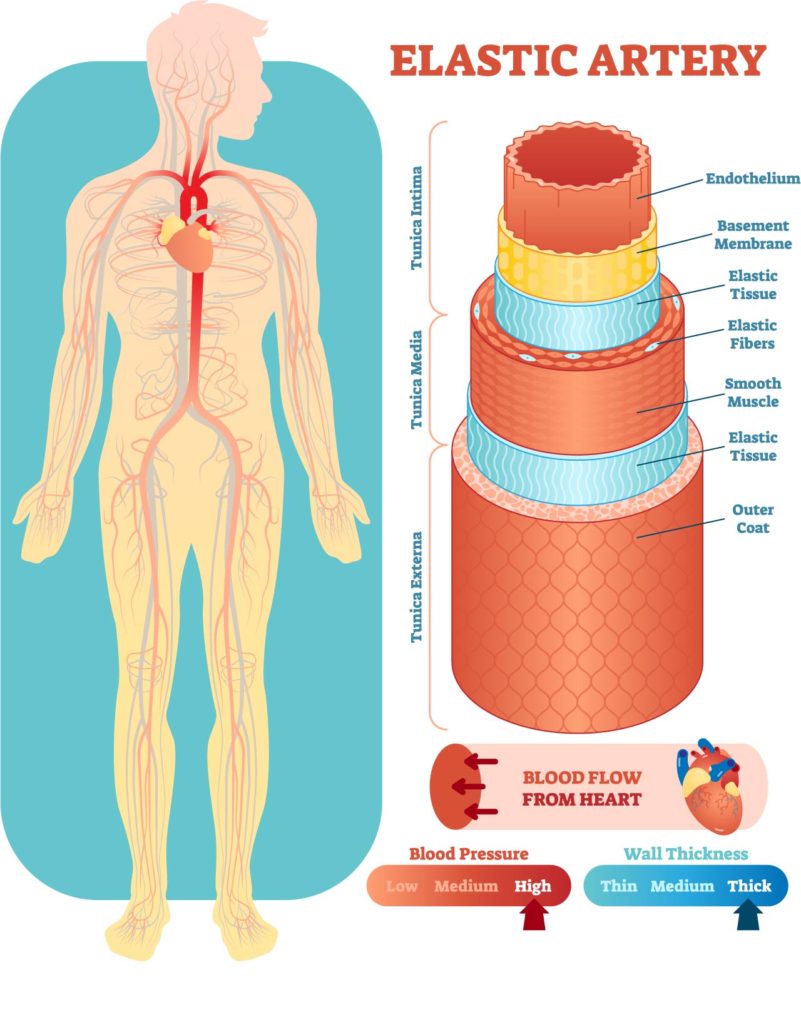
The image provides an educational overview of the structure and function of an elastic artery within the human circulatory system. On the left side, we see a simplified diagram of the human body with the heart and major arteries highlighted in red, indicating the pathway of oxygenated blood flow from the heart to various parts of the body.
The right side of the image offers a detailed cross-section of an elastic artery, which is one of the large vessels that lead directly from the heart. This type of artery is equipped to handle high pressure and large volumes of blood pumped by the heart. The cross-section is divided into several layers, each with a specific function:
- The innermost layer is the endothelium, a smooth lining that reduces friction and allows blood to flow freely.
- Next is the basement membrane, which provides physical support for the endothelial cells.
- The middle layers contain elastic tissue and elastic fibers, giving the artery its characteristic ability to stretch and recoil with each heartbeat, aiding in maintaining blood pressure and flow.
- Surrounding the elastic tissue are layers of smooth muscle, which can contract or relax to change the diameter of the artery, thus regulating blood pressure and flow.
- Finally, the outermost layer is the outer coat, which provides additional protection and structure to the artery.
At the bottom, two gauges indicate the relationship between blood pressure and wall thickness in arteries. The blood pressure gauge shows low, medium, and high levels, correlating with the wall thickness gauge directly below it, which shows thin, medium, and thick walls. This suggests that higher blood pressure requires thicker arterial walls to withstand the increased stress on the vessel.
This visual aid is an excellent tool for understanding the anatomy and physiology of arteries, particularly in how they accommodate and regulate the blood flow from the heart throughout the body.
Muscular Artery Anatomy
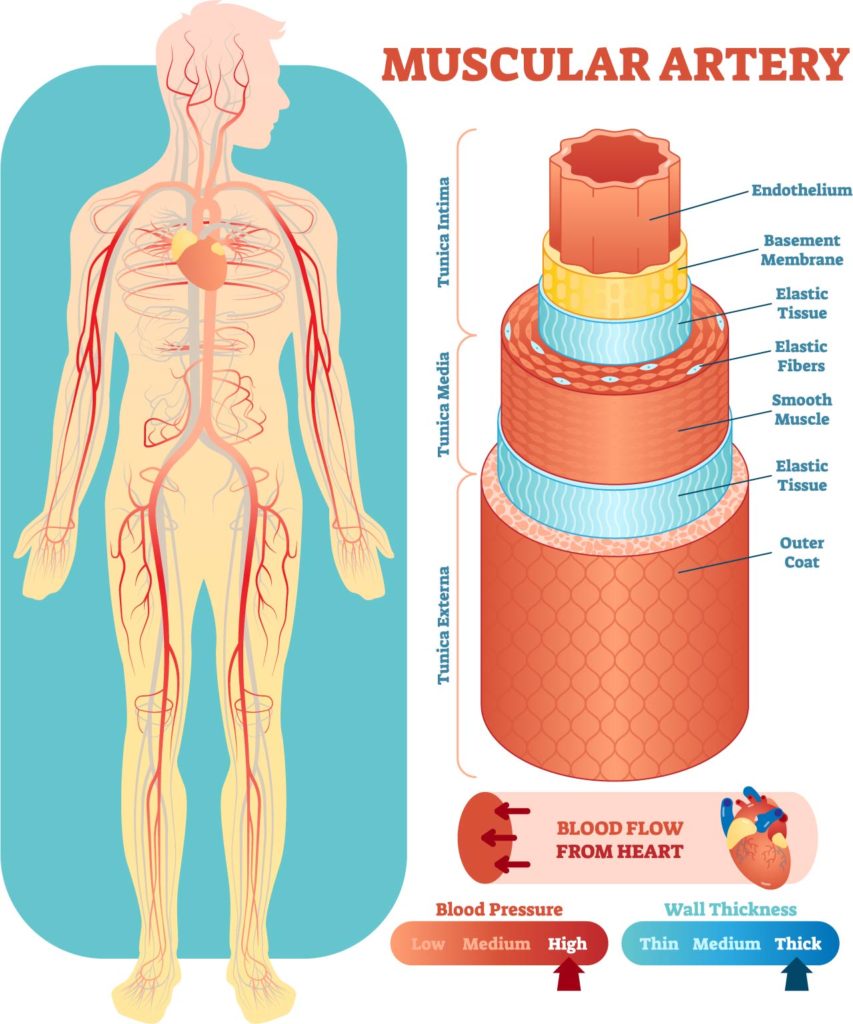
The image presents a visual representation of the circulatory system focusing on muscular arteries. It illustrates the human body with arteries depicted in red, highlighting the pathway of arterial blood flow from the heart to various regions of the body. Arteries are shown extending to the arms, the head, and down the legs, indicating the distribution of oxygen-rich blood throughout the body.
On the right side, there is an enlarged view of a muscular artery’s structure, showing various layers and components. The innermost layer is the endothelium, a smooth lining that keeps blood flowing freely. Surrounding the endothelium is the basement membrane, providing structural support. Next, there’s a layer of elastic tissue, allowing the artery to stretch in response to each pulse of blood. This is followed by a thick layer of smooth muscle, which can contract or relax to control the diameter of the artery. Another layer of elastic tissue follows, providing additional elasticity to the artery. The outermost layer, called the outer coat, serves as a protective sheath.
The graphic also includes indicators for blood pressure and wall thickness. It shows that blood pressure can be low, medium, or high, which correlates with the wall thickness of the arteries being thin, medium, or thick, respectively. These attributes are crucial for maintaining adequate blood flow and pressure throughout the circulatory system.
This informative image serves as an educational tool to understand the structure of arteries and how blood pressure and wall thickness can affect circulation. It demonstrates the essential role of arteries in transporting blood pumped by the heart to tissues and organs.
Continuous Capillary Anatomy
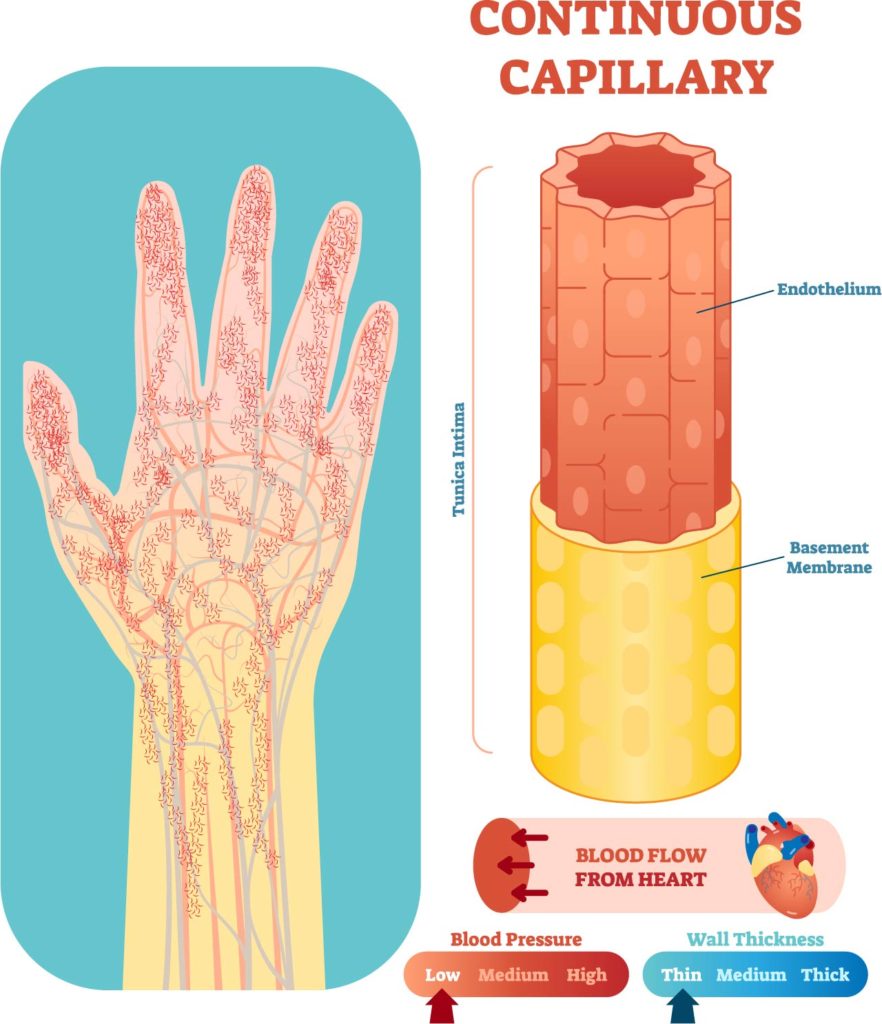
The image displays the intricacies of the capillary network within a human hand, as well as a detailed segment of a continuous capillary. The hand is shown with a complex web of fine capillaries branching out to supply blood to the entire hand, depicting the extensive reach of the body’s smallest blood vessels.
On the right, there’s an enlarged cross-sectional view of a continuous capillary, which is the most common type of capillary found throughout the body. It features the endothelium, a single layer of cells that forms the inner lining of the capillary, facilitating the exchange of water, oxygen, carbon dioxide, and many other nutrients and waste substances between blood and the surrounding tissues. Below the endothelium is the basement membrane, a supportive layer that provides structural stability.
The diagram also indicates the relationship between blood flow from the heart, blood pressure, and wall thickness in capillaries. Blood pressure is categorized as low, medium, or high, which corresponds to the capillary wall thickness, being uniformly thin across these categories. This thinness is essential for the exchange of materials between the blood and tissues.
Capillaries, especially the continuous type shown here, are critical in the circulatory system as they allow for this direct exchange with tissue cells, providing them with nutrients and oxygen while taking away metabolic waste. The visualization serves to highlight the fundamental role of capillaries in the microcirculation within the body’s tissues.
Capillary Anatomy
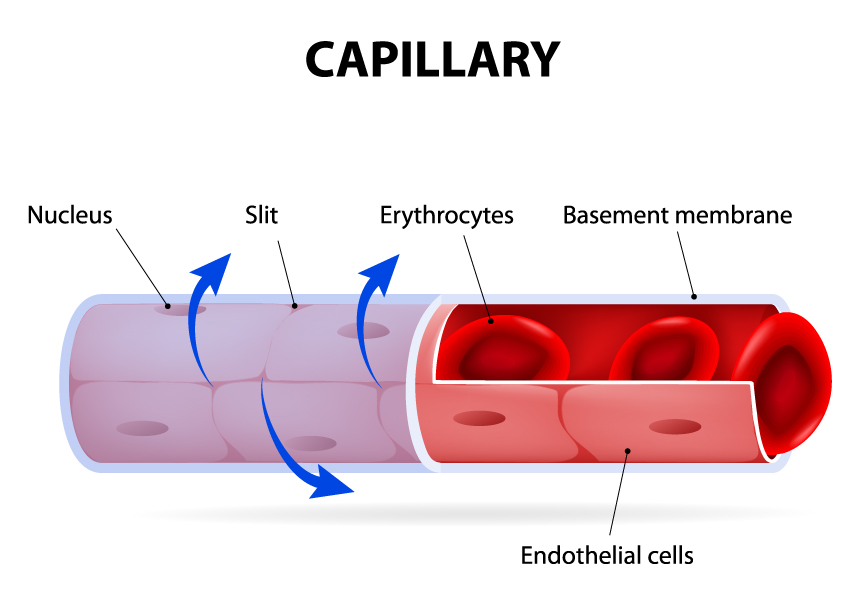
This image provides a detailed look at the structure of a capillary, the smallest of the body’s blood vessels. It’s a cross-sectional view that shows the capillary wall and its contents.
The capillary wall is composed of endothelial cells, which are long and thin to facilitate the exchange of substances between the blood and surrounding tissues. These cells line the inner surface of the capillary. The nuclei of the endothelial cells are visible, indicating the location of each cell’s genetic material. This is important because the nucleus controls the activity of the cell, including the transfer of substances.
Slits between the endothelial cells are also shown. These small openings or intercellular clefts allow certain molecules to pass through, playing a critical role in the selective exchange of substances between the blood and the interstitial fluid surrounding the body’s cells.
Inside the capillary, erythrocytes, or red blood cells, are depicted. Erythrocytes are responsible for carrying oxygen from the lungs to the body’s tissues and returning carbon dioxide to the lungs for exhalation. Their biconcave shape increases the surface area for gas exchange and allows them to deform as they pass through the narrow capillaries.
Beneath the endothelial cells lies the basement membrane, a thin layer of extracellular matrix that provides structural support to the capillary. It filters substances that pass in and out of the blood and contributes to the selective permeability of the vessel wall.
The illustration effectively demonstrates the basic structure of capillaries and highlights their role in microcirculation, where the exchange of gases, nutrients, and waste products occurs between the blood and tissues.
Baroreceptor Reflex
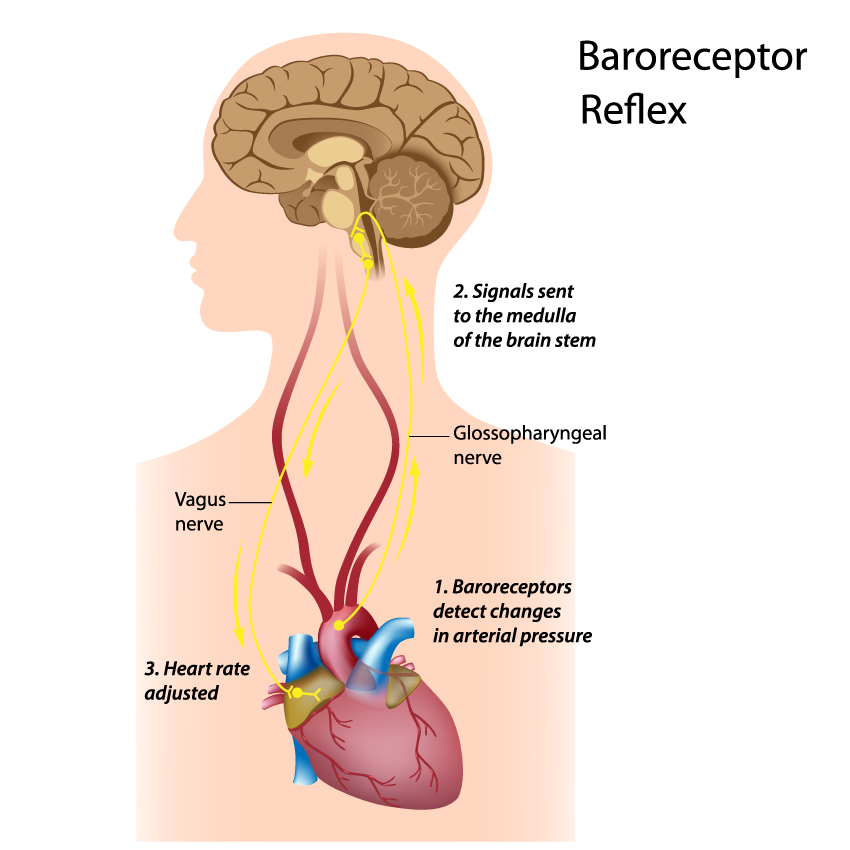
The image details the baroreceptor reflex, a critical feedback mechanism that helps maintain blood pressure at nearly constant levels within the human body.
At the bottom of the image is the heart, labeled with the step “3. Heart rate adjusted.” This indicates the final step in the baroreceptor reflex pathway, where the heart adjusts its rate in response to signals it receives, either increasing or decreasing the heart rate to raise or lower blood pressure accordingly.
Leading up from the heart are two nerves. The vagus nerve, extending from the heart to the brain, is known to mediate the parasympathetic response that can decrease the heart rate. The glossopharyngeal nerve is also shown, and it is associated with transmitting sensory information, including blood pressure information from the baroreceptors.
The baroreceptors themselves, mentioned in step “1. Baroreceptors detect changes in arterial pressure,” are not explicitly shown but are typically located in the walls of the carotid sinuses and the aortic arch. They are sensitive to the pressure of the blood flowing through these vessels.
The second step, “2. Signals sent to the medulla of the brain stem,” refers to the process where the baroreceptors send the blood pressure information through the glossopharyngeal and vagus nerves to the medulla oblongata, part of the brain stem. The medulla oblongata then processes these signals and initiates the appropriate autonomic response to regulate blood pressure.
The brain is depicted at the top of the image, indicating the destination of the signals transmitted by the nerves. It is the control center that integrates the baroreceptor information and modulates the cardiovascular system accordingly.
This reflex is vital for the short-term regulation of blood pressure, ensuring that sufficient blood flow is maintained to the brain and other vital organs. The image simplifies this complex physiological process into a clear sequence of events that illustrate how the body monitors and maintains stable blood pressure levels.
Coagulation Physiology
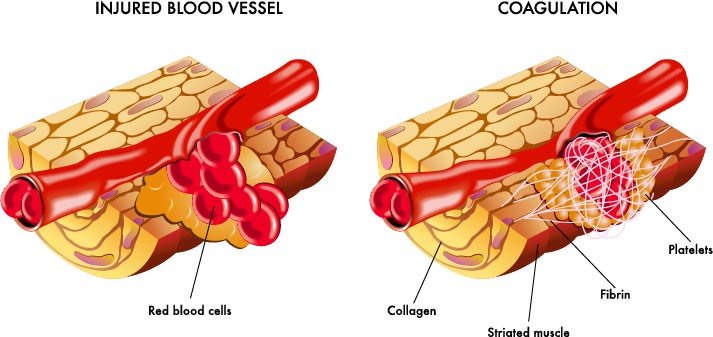
The image is a two-part illustration that explains the process of coagulation, which is the body’s mechanism to prevent excessive bleeding when a blood vessel is injured.
On the left side, under the label “INJURED BLOOD VESSEL,” we see a blood vessel that has been damaged. The vessel wall is torn, and red blood cells are shown escaping from the opening. The surrounding tissue includes striated muscle and collagen fibers, which provide structural support to the vessel. When a blood vessel is injured, the body exposes collagen fibers that are not normally in contact with blood flow.
The right side of the illustration, labeled “COAGULATION,” demonstrates the body’s response to the injury. The coagulation cascade has been activated, leading to the formation of a blood clot. This process involves the aggregation of platelets, which are small cell fragments in the blood that rush to the site of injury to form a temporary plug. The platelets adhere to the exposed collagen fibers and release chemicals that further activate clotting.
In addition to platelets, we see threads of fibrin, a protein involved in the clotting process. Fibrin forms a meshwork that traps red blood cells and platelets, creating a stable clot that seals the vessel to prevent further blood loss.
The two images together effectively demonstrate the initial response to vascular injury and the subsequent steps of hemostasis that the body employs to maintain the integrity of the circulatory system. This process is critical for survival, as it prevents excessive blood loss while the vessel wall repairs itself.
Atherosclerosis Pathology
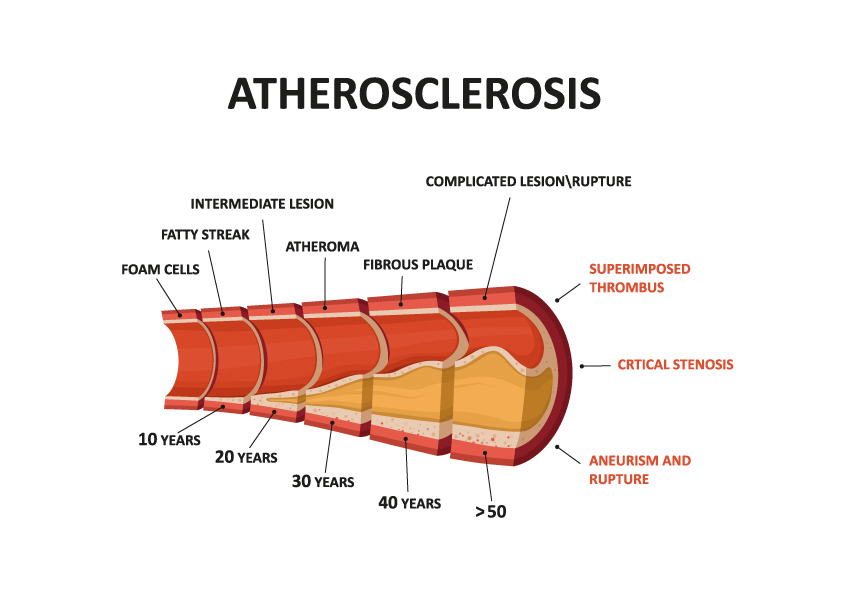
The image is an illustrative timeline of the progression of atherosclerosis, a chronic inflammatory response in the walls of arteries, largely due to the deposition of lipoproteins – cholesterol-containing particles that travel in the bloodstream.
At the earliest stage, depicted at approximately 10 years, “fatty streaks” are visible. These are the earliest visible lesions in the development of atherosclerosis and consist of lipid-laden foam cells. Foam cells are macrophages – a type of white blood cell – that have ingested low-density lipoproteins (LDL), commonly known as “bad cholesterol.”
As time progresses to 20 years, these fatty streaks evolve into “intermediate lesions.” At 30 years, the diagram shows “atheromas,” which are more advanced lesions characterized by the accumulation of lipids, inflammatory cells, smooth muscle cells, and connective tissue, forming a soft core with a fibrous cap, known as “fibrous plaque.”
By 40 years, the image shows that the fibrous plaque has thickened, which can lead to “critical stenosis,” a significant narrowing of the artery. The timeline suggests that at this stage, the artery’s ability to allow blood to flow is critically reduced, which can lead to ischemia – a restriction in blood supply to tissues.
After 50 years, the diagram indicates the possibility of “complicated lesion/rupture.” This is when the fibrous cap of the plaque ruptures, leading to the exposure of blood to the thrombogenic core material, which can result in the formation of a “superimposed thrombus” – a blood clot that forms on top of the ruptured plaque. This can completely block the artery or break free and cause a blockage elsewhere in the circulatory system, potentially leading to a heart attack or stroke.
The image also indicates “aneurism and rupture” as a potential outcome in advanced stages. An aneurysm is an abnormal bulge in the wall of an artery that can grow over time and may eventually rupture, causing life-threatening bleeding.
This visualization educates on how atherosclerosis can silently progress over decades and underscores the importance of preventive measures and monitoring for cardiovascular health.
Plaque Formation
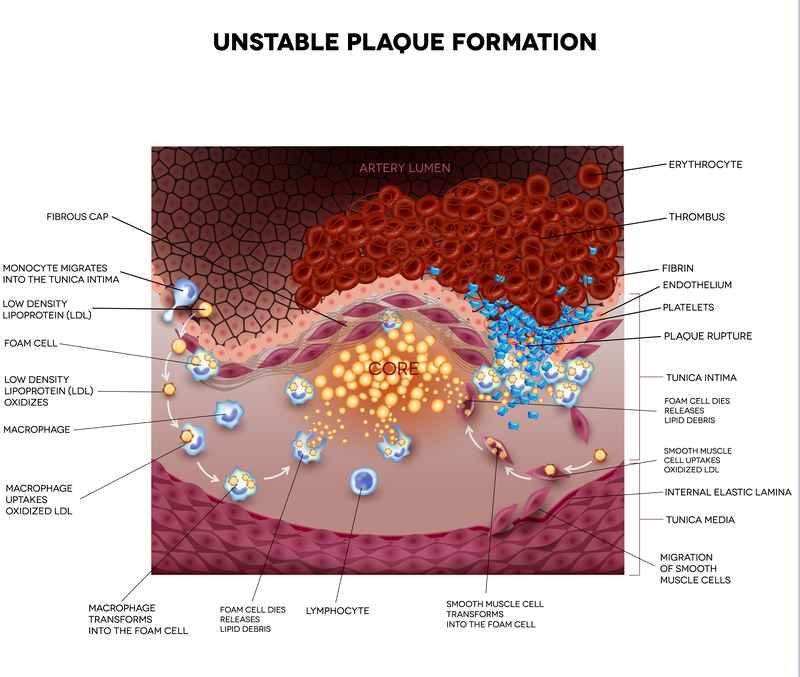
The image depicts the complex process of unstable plaque formation within an artery, a condition that can lead to serious cardiovascular events. The cross-section of the artery shows various elements involved in the development of an atherosclerotic plaque and its potential consequences.
At the top, the “fibrous cap” is a layer of connective tissue that covers the atheromatous core of the plaque. The stability of this cap is crucial as its rupture can lead to the formation of a thrombus (blood clot).
Beneath the fibrous cap is the “core” of the plaque, containing cholesterol crystals, foam cells, and other cellular debris. Foam cells are formed when macrophages ingest low-density lipoproteins (LDL), which are then oxidized within these cells. This process is shown through arrows indicating monocytes migrating into the intima (innermost layer of the artery wall), transforming into macrophages, and subsequently into foam cells.
Also illustrated are “lymphocytes,” a type of white blood cell involved in the inflammatory response, and “smooth muscle cell migration,” where smooth muscle cells from the media layer move into the intima.
Within the artery lumen, “erythrocytes” or red blood cells are shown flowing through the vessel. Near the site of plaque rupture, a “thrombus” is forming, consisting of fibrin (a fibrous protein involved in clot formation), endothelium (the inner lining of the blood vessel), and platelets (small blood cells that help with clotting).
The “tunica intima” is the innermost layer of the artery, under the endothelium, and is where the atherosclerotic plaque primarily forms. The “tunica media” is the middle layer composed of smooth muscle cells and the “internal elastic lamina,” a thin layer of elastic fibers that provides structural support and elasticity to the artery.
The process of plaque formation and rupture is a dynamic and potentially dangerous one, as it can significantly hinder blood flow or lead to the detachment of the thrombus, causing a blockage downstream, which is a primary mechanism leading to heart attacks and strokes. This detailed illustration aids in understanding the pathophysiology behind atherosclerotic cardiovascular diseases.
Anatomical Terms and Definitions
| Term | Definition |
|---|---|
| Aneurysm | An abnormal bulge in the wall of an artery that can grow over time and may eventually rupture, causing life-threatening bleeding. |
| Angioplasty | A medical procedure used to widen narrowed or obstructed arteries, typically to treat arterial atherosclerosis. |
| Arteries | Blood vessels that carry oxygen-rich blood from the heart to various parts of the body. |
| Atherosclerosis | A chronic inflammatory response in the walls of arteries, largely due to the deposition of lipoproteins (cholesterol-containing particles). |
| Baroreceptor Reflex | A critical feedback mechanism that helps maintain blood pressure at nearly constant levels within the human body. |
| Basement Membrane | A layer that provides physical support for endothelial cells and contributes to the selective permeability of vessel walls. |
| Blood Clot | A mass formed by the aggregation of platelets and fibrin in the blood to stop bleeding. |
| Capillaries | The smallest blood vessels in the body, facilitating the exchange of water, oxygen, carbon dioxide, and other nutrients and waste substances between blood and surrounding tissues. |
| Coagulation | The body’s mechanism to prevent excessive bleeding when a blood vessel is injured, involving the activation of a cascade that leads to the formation of a stable blood clot. |
| Continuous Capillary | The most common type of capillary, characterized by a continuous endothelial layer, facilitating exchange between blood and tissues. |
| Elastic Artery | A large vessel that leads directly from the heart, equipped to handle high pressure and large volumes of blood, characterized by its ability to stretch and recoil. |
| Endothelium | The innermost lining of blood vessels, providing a smooth surface that reduces friction and allows blood to flow freely. |
| Erythrocytes | Red blood cells responsible for carrying oxygen from the lungs to the body’s tissues and returning carbon dioxide to the lungs for exhalation. |
| Fatty Streaks | The earliest visible lesions in the development of atherosclerosis, consisting of lipid-laden foam cells. |
| Fibrous Plaque | An advanced atherosclerotic lesion characterized by a lipid core, inflammatory cells, smooth muscle cells, and a fibrous cap. |
| Foam Cells | Macrophages that have ingested low-density lipoproteins (LDL), becoming lipid-laden and contributing to the formation of atherosclerotic plaques. |
| Intercostal Arteries | Branching vessels from the thoracic aorta that supply blood to the ribs, chest wall, and muscles between the ribs. |
| Intima | The innermost layer of an artery or vein, consisting of endothelial cells and a thin layer of connective tissue. |
| Muscular Artery | A type of artery with a thick layer of smooth muscle in its wall, capable of contracting or relaxing to regulate blood flow and pressure. |
| Plaque | An accumulation of lipids, cholesterol, and other substances on the arterial wall, leading to atherosclerosis. |
| Smooth Muscle | Muscle found in the walls of arteries that can contract or relax to change the diameter of the artery, thus regulating blood pressure and flow. |
| Stent | A small wire mesh tube used to keep an artery open after an angioplasty procedure. |
| Thrombus | A blood clot that forms in a vessel and remains there, potentially leading to vascular obstruction. |
| Tunica Media | The middle layer of an artery or vein, composed of smooth muscle cells and elastic fibers, providing structural support and elasticity. |
| Unstable Plaque | A type of atherosclerotic plaque with a thin fibrous cap that is prone to rupture, leading to the formation of a thrombus and potentially causing a heart attack or stroke. |

