We use the term “superficial” to mean “situated or occurring on the skin or immediately beneath it” (Dictionary.com). In our work with tuning forks and VFRT, we find most of the pain points and mobility restrictions in the outer superficial and deep layers above the muscle and tendon layers. It is within these layers were biology and science in general has overlooked or ignored some of the pathology and issues residing in these outer layers. We give the solid part of fascia collagen fibers such a large spotlight, but the overall story is missing a co-lead character called interstitial fluid. When this fluid occupies the fatty layers there is a chance for big problems when the fluid separates from the proteoglycan gel within the layer. Then the pressure created by the pressurized fluids presses against pain receptors and restricts mobility in all layers in the local area.
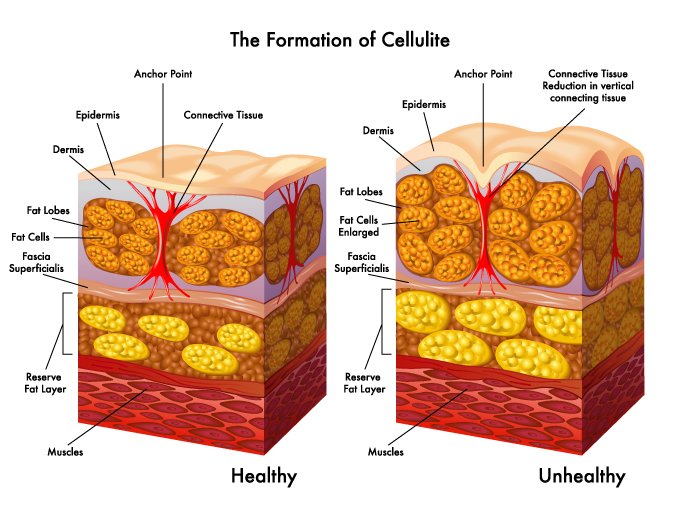
In the first image, we can see the layers of our tissue from the surface (epidermis) down to the superficial adipose (fat) layer where the fat cells are separated into larger sacks called lobules. This layer of fat is known as White Adipose Tissue (WAT). Below the superficial adipose layer is a series of collagen fiber sheets called superficial fascia. These sheets are designed to slide back and forth across each other during movement. Below the superficial fascia layer(s) is the deep adipose layer with a slightly different type of fat called brown adipose tissue (BAT) and is known as a reserve fatty layer. Below the deep adipose layer is more fascial sliding sheets and the outer fascial wrapping around the muscles. We can see these two adipose layers in the image below where we conducted a study of cow tissue. The tissue with the hair attached is the outer white adipose tissue or superficial adipose layer and the tissue on the left side is the deeper adipose layer or brown adipose tissue.

In the first image, we can also see vertical bundles of collagen fibers labeled as Anchor Points. These anchors are known as retinaculum cutis superficialis on the outer superficial adipose layer. These anchors are designed to keep the skin from stretching too far in any direction which could cause physical damage to our vessels and nerves running through those spaces. The right side of the first image shows how the anchors can start to shrink in length over time while the size of our fat cells can increase as we gain more weight. These two things will translate to the surface of the skin as cellulite. There is no magic substance underneath the skin known as cellulite, but it’s more of a condition brought on by a reduction in fluid intake and an increase in fat storage.

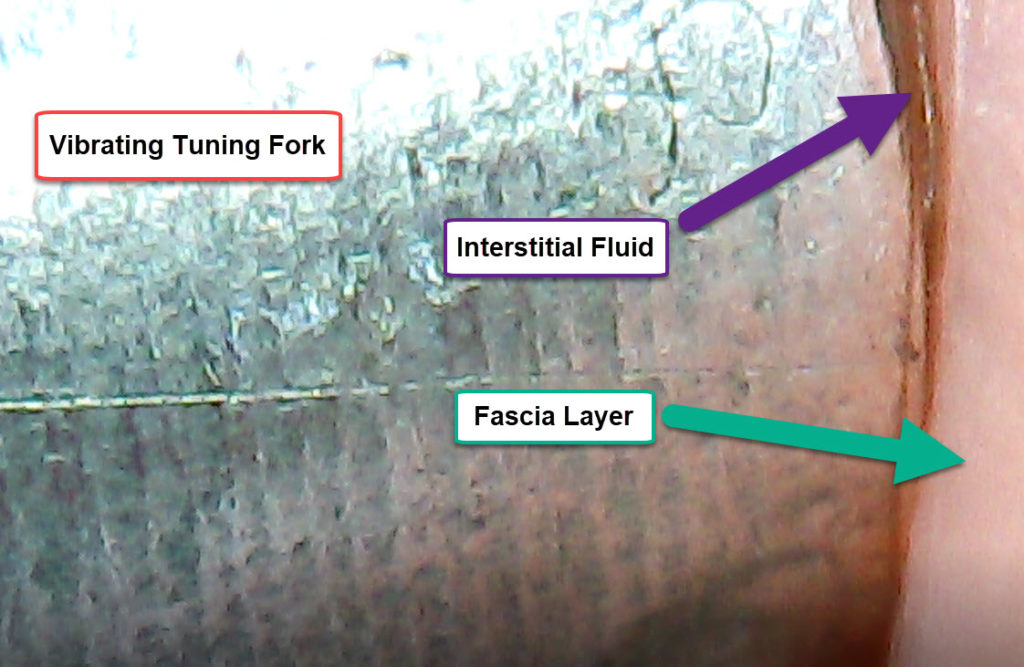
It has been well known and documented in the past that we cannot get rid of cellulite, but then we didn’t consider tuning forks as a possible resolution for targeted fat cell release. In the image above, we can see the base of a tuning fork pressed against fat cells which releases the lipids back into the interstitial space as the vibration allows for fluid diffusion across layers of fascia. We also see the same thing with pressurized fluids in the same space where the tuning forks will drain fluids from one layer (image below) to another thereby releasing the fluid pressure on nerve endings, decompressing cardiovascular vessels, and allowing lymphatic vessels to remove excess fluids from the interstitial space.
Vibration from a tuning fork has been the missing ingredient for most clinical methods and resolution of most conditions. Several research papers and books on fascia state that both pressure (or stretch) AND vibration are required for changes to the cells and tissue. For example, in the book Fascia -- What it is and why does it matter, we see in a section discussing mechanotransduction with integrins used to communicate between the Extra-cellular matrix of collagen fibers that the integrins “are sensitive to both stretch and vibration. It is as if each cell in the body was plugged into the ECM so that it can also monitor the environment by listening to it. When the integrin is stimulated, it responds by creating electrochemical changes at the cellular level. The process of creating change via mechanical pressure and vibration at the cellular level.” (Lesondak, David. Fascia -- What is is and why it matters (p. 12). Handspring Pub Ltd. Kindle Edition.)
We can also see the same pressure and vibration example used to describe the way fascia collagen fibers respond and remodel.
“So, fascia responds according to mechanical supply and demand, and follows Wolff’s law. Fibroblasts are both spooling out more collagen where necessary and secreting collagenase, a collagen-eating enzyme, all based on signals of pressure and vibration, like a cellular public works department – building, knocking down, and cleaning up the collagen matrix.” (p. 14).
Knowing these things about pressure and vibration, it often makes me wonder why tuning forks and vibration has been left out of the possible clinical methods involved in alternative and complementary medicine. VFRT is based on this premise of pressure and vibration along with a deep understanding of the fluid pressure and fascial restrictions unable to remodel. We look at the outer layers instead of the musculo-skeletal layers where most fascia release methods are focused.