The various mechanisms of dysfunction in the liver
The liver, a vital organ in the human body, can be affected by various mechanisms of dysfunction, leading to a wide range of liver diseases and conditions. These mechanisms can be broadly categorized into several key areas:
Infectious Causes:
- Viral Hepatitis: Hepatitis A, B, C, D, and E are viruses that primarily affect the liver, causing inflammation, damage, and impaired liver function.
- Other Infections: Parasitic infections like schistosomiasis or bacterial infections can also impact liver function.
Toxic Insults:
- Alcohol Abuse: Chronic alcohol consumption can lead to alcoholic liver disease, including fatty liver, alcoholic hepatitis, and cirrhosis.
- Drug-Induced Liver Injury: Certain medications, herbal supplements, and toxins can cause liver damage, ranging from mild elevation in liver enzymes to severe liver failure.
Metabolic and Genetic Disorders:
- Non-Alcoholic Fatty Liver Disease (NAFLD) and Non-Alcoholic Steatohepatitis (NASH): These conditions are related to metabolic syndrome and are characterized by the accumulation of fat in the liver.
- Hemochromatosis: A genetic condition leading to excessive iron accumulation in the liver.
- Wilson’s Disease: A rare genetic disorder causing abnormal copper accumulation in the liver.
- Alpha-1 Antitrypsin Deficiency: A genetic disorder that can lead to liver damage.
Autoimmune Disorders:
- Autoimmune Hepatitis: The immune system attacks liver cells, causing inflammation and damage.
- Primary Biliary Cholangitis (PBC) and Primary Sclerosing Cholangitis (PSC): These are autoimmune conditions that affect the bile ducts within and outside the liver.
Vascular Abnormalities:
- Budd-Chiari Syndrome: Obstruction of the liver veins leading to liver congestion and damage.
- Portal Hypertension: High blood pressure in the portal vein system, often due to cirrhosis, leading to complications like varices and ascites.
Biliary Tract Diseases:
- Cholestasis: Impairment of bile flow which can be due to various causes, including gallstones, strictures, or tumors.
- Gallstones: Can block the bile ducts, causing inflammation and biliary colic.
Tumors and Cancers:
- Hepatocellular Carcinoma (HCC): The most common type of primary liver cancer.
- Metastatic Cancers: Cancers from other sites can also spread to the liver.
Lifestyle Factors:
- Obesity and Poor Diet: These factors contribute significantly to the development of NAFLD and NASH.
- Lack of Exercise: Sedentary lifestyle can exacerbate the risk of metabolic liver diseases.
Each of these mechanisms can lead to liver dysfunction in different ways, affecting the liver’s ability to perform its essential functions, including detoxification, protein synthesis, and metabolism. Early detection and management of liver diseases are crucial for preventing progression to more severe conditions such as liver cirrhosis or liver failure.
Progressive liver dysfunction due to chronic inflammation
Chronic inflammation in the liver, regardless of its underlying cause, can lead to a cascade of changes and damage within the liver tissue. This process can progress through several stages, ultimately impacting the liver’s ability to function properly. Here’s an overview of what happens:
- Persistent Inflammation: Chronic inflammation means that the liver is continuously exposed to inflammatory cells and cytokines. This ongoing inflammatory response can be due to various reasons, such as long-term alcohol abuse, chronic viral hepatitis, autoimmune diseases, metabolic disorders like NAFLD and NASH, or toxic substances.
- Cellular Damage: The inflammatory process damages hepatocytes (liver cells), leading to cell death and tissue injury. This damage can trigger further inflammation, creating a vicious cycle.
- Fibrosis: One of the liver’s responses to chronic injury is to attempt to repair itself. This repair process involves the activation of stellate cells, which then produce collagen and other extracellular matrix proteins. Over time, this results in the accumulation of fibrous tissue in the liver, a process known as fibrosis.
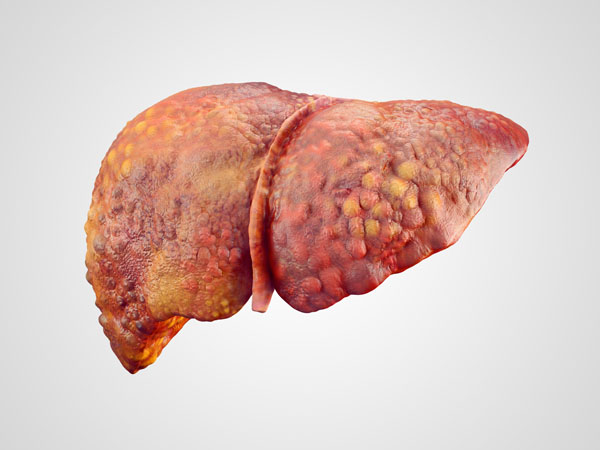
- Cirrhosis: As fibrosis progresses, it can lead to cirrhosis, where the normal liver architecture is replaced by scar tissue (fibrotic tissue) and regenerative nodules. Cirrhosis is characterized by a distortion of the liver’s normal structure and vasculature, leading to significant impairment in liver function.
- Impaired Liver Function: With the progression of cirrhosis, the liver’s ability to perform its vital functions is increasingly compromised. These functions include detoxification of harmful substances, synthesis of essential proteins like albumin and clotting factors, metabolism of fats and carbohydrates, and processing of nutrients absorbed from the intestine.
- Portal Hypertension: The distortion of liver architecture and the increased fibrosis can lead to increased resistance to blood flow through the liver. This results in elevated pressure in the portal vein, known as portal hypertension. Portal hypertension can lead to serious complications, such as the development of varices (abnormally enlarged veins) and ascites (fluid accumulation in the abdomen).
- Decreased Immune Function: The liver plays a role in immune surveillance. Chronic liver disease can impair this function, making the body more susceptible to infections.
- Liver Failure: In advanced stages, chronic liver disease can lead to liver failure, a life-threatening condition where the liver loses its ability to function. This can result in jaundice, coagulopathy (bleeding disorders), encephalopathy (brain dysfunction), and multiple organ failure.
- Risk of Liver Cancer: Chronic liver inflammation and cirrhosis significantly increase the risk of developing hepatocellular carcinoma, a type of liver cancer.
Overall, chronic inflammation in the liver can lead to a progressive decline in liver function, serious complications, and an increased risk of liver cancer. Early detection and management of the underlying cause of inflammation are critical to prevent or slow down these adverse outcomes.
The liver’s protective membrane
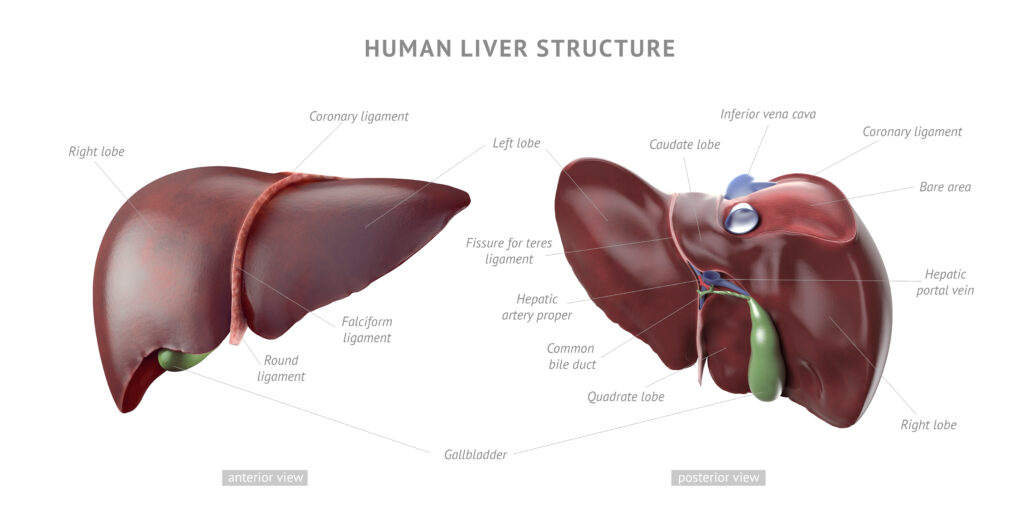
The liver, one of the largest organs in the body, is surrounded by a thin, protective membrane known as the Glisson’s capsule. This capsule plays several important roles in the structure and function of the liver:
- Composition: Glisson’s capsule is primarily composed of connective tissue, which includes a mixture of collagen fibers and elastin. This composition provides both strength and elasticity to the membrane, allowing it to protect the liver while accommodating its movements and changes in size during digestion and other metabolic activities.
- Protection: The primary function of Glisson’s capsule is to protect the liver from physical damage. It acts as a barrier, safeguarding the liver against mechanical injuries and external shocks.
- Structural Framework: The capsule provides a structural framework for the liver. It extends into the liver, forming a fine, supportive network that helps maintain the shape and architecture of the organ.
- Vascular and Biliary Support: Glisson’s capsule also envelops the hepatic artery, portal vein, and bile ducts as they enter the liver. This encapsulation is important for the stability and protection of these vessels and ducts.
- Innervation: The capsule is sensitive to distension and pain, as it contains nerve endings. In conditions where the liver is swollen, such as in hepatitis or congestion, the capsule can stretch, leading to pain or discomfort.
- Inflammation Response: In certain liver diseases, such as hepatitis or cirrhosis, the Glisson’s capsule can become inflamed. This inflammation can contribute to the pain and discomfort associated with these conditions.
Overall, Glisson’s capsule is a crucial component of liver anatomy, providing protection, structural integrity, and support for vascular and biliary structures within the liver. Its role becomes especially evident in pathological conditions where changes in the liver’s size or structure can lead to symptoms arising from the capsule itself.
How can a membrane become inflamed without a blood supply?
Glisson’s capsule, while it does not have a robust blood supply of its own, is still capable of becoming inflamed due to its close proximity to the liver’s extensive vascular network and its own sensory nerve fibers. Inflammation of the Glisson’s capsule is often a secondary response to underlying liver conditions. Here’s how it can occur:
- Proximity to Liver Tissue: Glisson’s capsule is directly adhered to the liver tissue. If the liver becomes inflamed or injured (for example, in hepatitis, cirrhosis, or liver congestion), the inflammation can extend to the capsule. The liver’s blood vessels, which are abundant and highly active, can release inflammatory mediators that affect the capsule.
- Transmission of Inflammatory Mediators: Inflammatory processes in the liver can lead to the production and release of various chemical mediators such as cytokines, prostaglandins, and other inflammatory molecules. These mediators can diffuse into the Glisson’s capsule, leading to an inflammatory response in the capsule itself.
- Nerve Stimulation: Glisson’s capsule is innervated by sensory nerves that can become activated by the stretching or distortion of the capsule, often a result of liver swelling. This nerve stimulation can result in pain and is often interpreted as inflammation.
- Secondary Inflammation Response: While the capsule doesn’t have its own blood supply, the inflammatory response is not solely dependent on direct blood supply to the affected area. The inflammatory cells and mediators can migrate from adjacent liver tissues to the capsule.
Inflammation of the Glisson’s capsule is typically a reactive process secondary to liver inflammation or damage. The close anatomical and functional relationship between the liver and its capsule facilitates this secondary inflammatory response, even in the absence of a direct blood supply to the capsule itself.
How inflammatory fluid progresses in liver dysfunction
The progression of liver dysfunction due to inflammation involves complex interplays between inflammatory processes, fluid dynamics, and pressure changes in and around the liver. Here’s a detailed explanation focusing on fluid accumulation, pressurization, and their impact on liver structures such as Glisson’s capsule and the development of ascites.
Initial Inflammatory Response:
- Inflammation in the liver, regardless of the cause, leads to the activation of immune cells and the release of inflammatory mediators like cytokines.
- These mediators increase the permeability of blood vessels, allowing more plasma to leak into the liver tissue. This results in swelling or edema within the liver.
Fluid Accumulation and Increased Pressure:
- As fluid accumulates, it increases the pressure within the liver. This is particularly significant in the liver due to its encapsulation by Glisson’s capsule.
- Glisson’s capsule, being a relatively non-distensible membrane, limits the expansion of the liver, contributing to increased tissue pressure when the liver swells.
- The increased intrahepatic pressure due to swelling can compress intrahepatic blood vessels, potentially impairing blood flow within the liver.
Impaired Hepatic Function:
- Elevated intrahepatic pressure and reduced blood flow can lead to hypoxia (reduced oxygen supply) and further damage to liver cells.
- The liver’s ability to process and remove toxins, synthesize proteins, and regulate metabolism is compromised.
Portal Hypertension:
- Chronic liver inflammation and subsequent scarring (fibrosis) can lead to increased resistance to blood flow through the liver, causing portal hypertension.
- Portal hypertension exacerbates fluid leakage into the abdominal cavity, leading to ascites.
Development of Ascites:
- Ascites, the accumulation of fluid in the peritoneal cavity, occurs due to a combination of high blood pressure in the portal vein and low levels of albumin (a protein made by the liver).
- Low albumin levels decrease the osmotic pressure of the blood, facilitating the transudation of fluid into the abdominal cavity.
Further Complications:
- Ascites itself can be uncomfortable and can lead to abdominal distension, respiratory difficulty, and increased risk of infections like spontaneous bacterial peritonitis.
- The elevated pressure in the abdominal cavity can also impair kidney function, a condition known as hepatorenal syndrome.
Progressive Deterioration:
- Ongoing inflammation, fibrosis, and increased pressure within the liver and abdominal cavity contribute to a progressive decline in liver function.
- This can eventually lead to cirrhosis and liver failure if the underlying causes are not addressed.
Compartmental Pressurization and Fluid Dynamics:
- The concept of compartmental pressurization is crucial in understanding the progression of liver disease. Increased pressure within the liver (due to inflammation and Glisson’s capsule constraints) and the abdominal cavity (due to ascites) alters the dynamics of fluid movement and pressure gradients, further complicating the clinical picture.
In summary, the progression of liver dysfunction from an inflammatory standpoint involves a complex interaction of immune responses, fluid dynamics, and pressure changes. The encapsulation of the liver by Glisson’s capsule and the development of ascites are key factors that contribute to the altered physiology in liver diseases. Managing these aspects is crucial in the treatment of liver disorders, especially in mitigating the complications arising from fluid accumulation and pressurization.
How does this progression of inflammatory fluids apply to a single dysfunction like cirrhosis?
The progression of fluid pressure due to inflammation in the context of cirrhosis is a multifaceted issue, involving more than just biochemical changes or fascial restrictions. Here’s a summary that encapsulates the complexity of this condition:
- Cirrhosis and Chronic Inflammation:
- Cirrhosis, often a result of long-standing liver inflammation, leads to the replacement of healthy liver tissue with scar tissue (fibrosis) and regenerative nodules.
- This process disrupts the normal architecture and function of the liver.
- Biochemical Alterations:
- The liver plays a crucial role in synthesizing proteins, including albumin, which helps maintain oncotic pressure (the pressure exerted by proteins) in the blood. Cirrhosis impairs this function, leading to decreased albumin levels.
- Lowered albumin levels reduce the blood’s oncotic pressure, facilitating the movement of fluid from blood vessels into surrounding tissues (edema).
- Hemodynamic Changes:
- Cirrhosis causes increased resistance to blood flow through the liver, leading to portal hypertension (elevated pressure in the portal vein).
- Portal hypertension exacerbates the transudation of fluid into the abdominal cavity, resulting in ascites.
- Impact of Glisson’s Capsule:
- Inflammation and fibrosis also involve Glisson’s capsule, which encases the liver.
- The non-expandable nature of Glisson’s capsule means that any swelling or increase in liver volume due to inflammation and fibrosis creates internal pressure within the liver.
- Fascial Considerations:
- While fascial restrictions may contribute to local pressure changes, the primary issue in cirrhosis is the pathological alteration of liver tissue and vasculature.
- The fascial tissue (Glisson’s capsule) around the liver is affected, but it’s more of a response to, rather than a cause of, the underlying liver pathology.
- Fluid Dynamics and Pressurization:
- The combination of decreased oncotic pressure (due to low albumin), increased hydrostatic pressure (from portal hypertension), and resistance from Glisson’s capsule leads to abnormal fluid dynamics and pressurization.
- This results in fluid accumulating in the liver (contributing to liver enlargement and pain) and in the abdominal cavity (ascites).
- Systemic Effects:
- Ascites can lead to increased abdominal pressure, affecting other organs and potentially leading to complications like hernias, respiratory issues, and renal impairment (hepatorenal syndrome).
- More Than Just Biochemical or Fascia:
- The progression of fluid pressure in cirrhosis is not solely a biochemical issue (protein synthesis) or a fascial problem (tissue constraints). It involves complex interactions between altered liver architecture, vascular changes, biochemical imbalances, and fluid dynamics.
- The systemic impact of these changes underscores the multifactorial nature of cirrhosis and its complications.
Cirrhosis and its related fluid pressure issues are the result of a combination of factors including tissue remodeling, vascular alterations, biochemical changes, and dynamic fluid shifts. This complexity necessitates a holistic approach in understanding and managing the condition.

