1208 Anatomy of Abdomen Organs
Smooth Muscle Tissue Video (53 secs):
Smooth muscle tissue is in the walls of hollow organs throughout the body. The tissue contracts and relaxes to contain substances and move substances through the body.
Smooth muscle contractions are involuntary actions managed by impulses that travel through the autonomic nervous system to the smooth muscle tissue.
The arrangement of cells in smooth muscle tissue provides for contraction and relaxation with great elasticity. The smooth muscle in the digestive tract contracts and relaxes in peristaltic waves that move swallowed food and nutrients from the mouth, through the stomach and the intestines. Artery walls include smooth muscle that relaxes and contracts as pressure changes move changing volumes of blood through the vessel. The smooth muscle of the bladder and uterus allow for contraction of those organs.
Peristalsis Video (53 secs):
Peristalsis is the wave-like action that propels food and chyme through the GI tract at the pace required for digestion and absorption.
The autonomic nervous system controls peristalsis by alternately contracting and relaxing the circular and longitudinal smooth muscle layers in the GI wall.
Peristalsis begins when the GI wall is distended and stimulated by the presence or imminent arrival of food or chyme. When the stomach and intestines, nervous or hormonal triggers increase both digestive mixing actions and the peristaltic waves.
Nutrition Absorption Video (1 min 1 sec):
Absorption occurs in the small and large intestines. It is facilitated by the pace and action of peristalsis, as well as the structure of the intestinal wall and its mucosa. In the small intestine, small peristaltic waves propel chyme gradually. Large, valvular folds called plica circularis swirl and slow chyme for absorption. Most absorption of nutrients from ingested food occurs through finger-like projections called villi. Inside each villus are lacteals and capillary beds, into which digestive products are passed.
The large intestine’s mucosal epithelium specializes in the absorption of ions and water. Haustral folds dig into chyme and expose remaining substances to mucosal walls.
Supporting Details:
The large intestine, also known as the colon, plays a crucial role in the final stages of digestion, especially in the absorption of water and electrolytes and the formation and expulsion of feces. Its anatomy is specialized to facilitate these functions. Here are the key features related to its role in processing chyme:
- Structure of the Large Intestine: The large intestine is roughly 1.5 meters (5 feet) in length and is divided into several parts: the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and anal canal.
- Mucosal Folds: Unlike the small intestine, which has villi and microvilli for absorption, the large intestine has a smoother lining. However, it does have folds known as haustra. These are sacculations caused by the contraction of the taeniae coli, which are longitudinal muscle bands on the colon.
- Role in Digestion: The large intestine doesn’t play a significant role in the chemical breakdown of food, but it’s crucial for absorbing water and electrolytes from the remaining indigestible food matter. The haustra facilitate this by slowing down the passage of chyme, allowing more time for water absorption.
- Interaction with Chyme: As the chyme enters the large intestine, it’s primarily liquid. The haustral contractions help to mix the chyme, exposing more of it to the mucosal walls where absorption occurs. The folds don’t “dig into” the chyme in a mechanical sense, but they do increase the surface area available for absorption and help in compacting the chyme into feces.
- Mucus Production: Goblet cells in the mucosa of the large intestine secrete mucus. This mucus lubricates the intestinal contents, aiding in the formation of feces and its passage through the rectum and anal canal.
- Microbial Activity: The large intestine houses a vast number of bacteria that aid in the fermentation of indigestible matter, producing gases and some additional nutrients like vitamin K, which are absorbed through the colonic walls.
- Rectum and Anal Canal: The final stages of waste processing occur in the rectum and anal canal, where feces are stored until they are expelled from the body through the process of defecation.
The large intestine’s anatomy, with its haustral folds and a simpler mucosal lining compared to the small intestine, is thus optimized for its primary roles in water absorption, fecal formation, and housing beneficial bacteria.
The term “plica circularis”:
These are large, valvular folds found in the small intestine, not the large intestine. They play a crucial role in digestion by increasing the surface area for absorption and helping to slow down the movement of chyme, allowing more time for nutrients to be absorbed. The plicae circulares are part of the small intestine’s internal structure, along with villi and microvilli, which further amplify the surface area for absorption. The villi are indeed finger-like projections, and each villus contains a network of capillaries, and a lymphatic vessel called a lacteal. Nutrients absorbed from the digested food pass into these capillaries and lacteals to be transported to other parts of the body.
Gall Bladder Video (29 secs):
Your gallbladder stores bile, a fluid made by your liver that aids in digestion. Gallstones are pieces of solid material that form in the gallbladder when substances in the bile harden. They range in size from a tiny speck to the size of a golf ball. Gallstones can block the flow of the fluid through the bile ducts. Signs of a gallstone attack may include nausea, vomiting, or pain in the abdomen, back, or just under the right arm.
More Details:
Gallstones are a common and often painful condition that occur when solid deposits form in the gallbladder, a small organ located just under the liver. To understand gallstones, it’s helpful to first understand the role of the gallbladder and bile in digestion:
Gallbladder and Bile
- Gallbladder: A small, pear-shaped organ located beneath the liver on the right side of the abdomen. Its primary function is to store and concentrate bile.
- Bile: A yellow-green fluid produced by the liver, essential for the digestion and absorption of fats in the small intestine. Bile contains water, cholesterol, fats, bile salts, proteins, and bilirubin.
Formation of Gallstones
- Composition: Gallstones can be composed of cholesterol, bilirubin (a breakdown product of red blood cells), and other components of bile. They are generally classified into two types:
- Cholesterol Stones: The most common type, usually yellow-green, and primarily made of hardened cholesterol.
- Pigment Stones: Smaller, darker stones made primarily from bilirubin.
- Causes: Gallstones form when substances in bile, particularly cholesterol or bilirubin, become too concentrated and harden. Factors contributing to gallstone formation include:
- Excess cholesterol in bile.
- Excess bilirubin in bile.
- Incomplete emptying of the gallbladder, which leads to bile becoming overly concentrated.
- Risk Factors: Certain conditions and lifestyles increase the risk of developing gallstones, such as:
- Being female.
- Being overweight or obese.
- Eating a high-fat or high-cholesterol diet.
- Rapid weight loss.
- Age (increased risk as people get older).
- Certain medical conditions like diabetes.
- Family history of gallstones.
Symptoms and Complications
- Symptoms: Many people with gallstones do not experience symptoms. However, if a gallstone blocks a bile duct, it can cause symptoms like:
- Sharp pain in the upper right or center of the abdomen.
- Nausea and vomiting.
- Fever, if an infection develops.
- Jaundice (yellowing of the skin and eyes).
- Complications: If left untreated, gallstones can lead to complications such as:
- Cholecystitis (inflammation of the gallbladder).
- Pancreatitis (inflammation of the pancreas).
- Cholangitis (inflammation of the bile ducts).
- Increased risk of gallbladder cancer (though rare).
Diagnosis and Treatment
- Diagnosis: Gallstones are often diagnosed through imaging tests such as ultrasound, CT scans, or MRIs.
- Treatment: Treatment depends on the severity of symptoms and may include:
- Surgery: The most common treatment is the surgical removal of the gallbladder (cholecystectomy), which is often performed laparoscopically.
- Medications: In some cases, medications to dissolve cholesterol gallstones may be used, though they are less effective and take a long time to work.
Gallstones and their associated symptoms can significantly impact quality of life. Understanding the risk factors and seeking prompt medical attention if symptoms occur is important for effective management and treatment of this condition.
Urinary Tract Video (42 secs):
The structures of the urinary system function to filter blood and remove waste from the body. The kidneys are the blood filtering organs. Blood enters the kidneys through the renal arteries. Within the kidneys, substances are filtered out of the blood into urinary structures. Some substances are then reabsorbed back into the blood and others are secreted into the urine. This three-step process cleans blood and creates the waste product urine. Urine exits the kidneys and moves down the ureters to the bladder.
As the bladder fills, interactions with the brain and nerves contract and relax muscular structures and urine is pushed out through the urethra in a process called micturition.
More Details:
The urinary system is a sophisticated network of organs and structures responsible for filtering blood, removing waste, and regulating various aspects of the body’s internal environment, such as fluid and electrolyte balance. Let’s delve into the functions of the urinary system, its primary components, and the process of urine formation and elimination, known as micturition.
Components of the Urinary System
- Kidneys: These are the primary organs of the urinary system. They filter blood, remove waste, regulate electrolytes, and maintain fluid balance. Blood enters the kidneys through the renal arteries, which branch off from the aorta.
- Ureters: These are muscular tubes that transport urine from the kidneys to the bladder. They use peristaltic waves (muscle contractions) to propel urine.
- Urinary Bladder: A hollow muscular organ that stores urine until it is ready to be expelled from the body. The bladder’s elasticity allows it to expand and accommodate varying volumes of urine.
- Urethra: The tube through which urine exits the body. In males, the urethra is also a part of the reproductive system as it carries semen out of the body.
Urine Formation
- Filtration: Occurs in the nephrons of the kidneys, where blood pressure forces water and solutes from the blood into the glomerular capsule, forming a filtrate.
- Reabsorption: As the filtrate passes through the nephron’s tubular system, essential substances like water, glucose, and certain ions are reabsorbed back into the bloodstream.
- Secretion: Additional waste substances and ions, not filtered out initially, are secreted from the blood into the tubular fluid.
Micturition (Urination)
- Bladder Filling: As the kidneys produce urine, it is collected in the bladder. As the bladder fills, it expands.
- Neural Interaction: When the bladder reaches a certain level of fullness, stretch receptors in its walls send signals to the brain, indicating the need to urinate.
- Urination Reflex: In response, the brain sends signals back to the bladder. Involuntary muscle contractions (in the bladder) and relaxation of the internal urethral sphincter occur. The external urethral sphincter, which is under voluntary control, must also relax to allow urine to pass.
- Urine Expulsion: Urine is expelled from the bladder through the urethra. This process can be consciously controlled to a significant extent in adults, allowing for the voluntary initiation or delay of urination.
Physiological Importance
- Waste Elimination: The primary function is to remove waste products, including urea, creatinine, and uric acid, from the bloodstream.
- Regulation of Blood Pressure and Volume: By controlling the amount of water and salts reabsorbed, the kidneys play a vital role in regulating blood pressure and blood volume.
- Electrolyte Balance: The kidneys help in maintaining the balance of various electrolytes like sodium, potassium, and calcium.
- Acid-Base Balance: The urinary system plays a crucial role in maintaining the pH balance of the blood.
Understanding the urinary system’s functions is essential in grasping how the body maintains homeostasis and the implications of urinary system-related disorders. This knowledge is fundamental in the medical field for diagnosing, managing, and treating various renal and urinary tract conditions.
Bladder Anatomy:
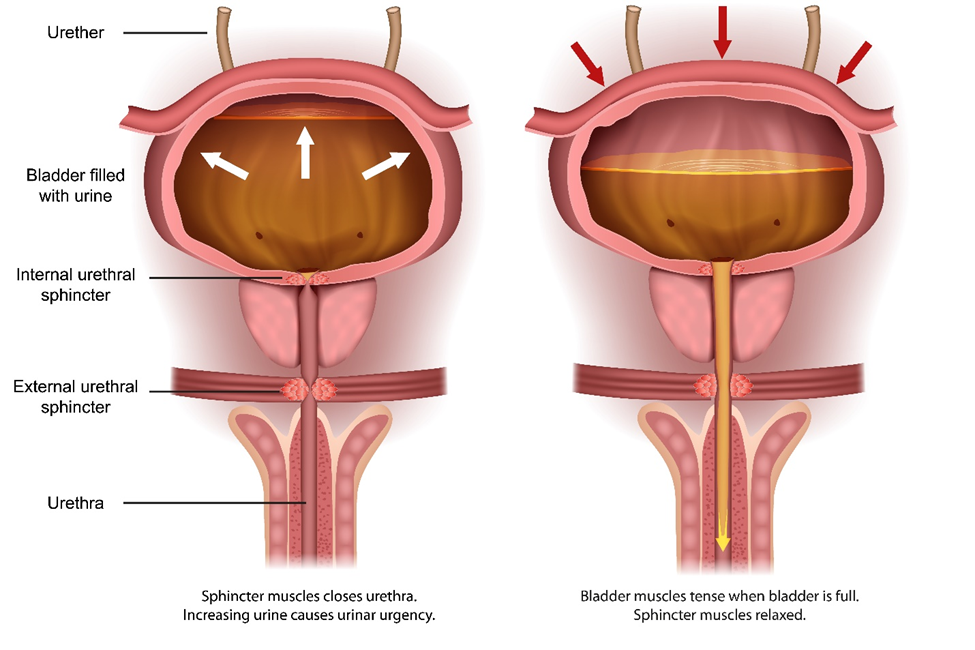
The image illustrates the urinary bladder in two different states: on the left, when it is filled with urine, and on the right, when it is in the process of emptying.
On the left side, the diagram shows the bladder full of urine, which is indicated by the white arrows pointing outwards, representing the expansion of the bladder. The internal urethral sphincter is closed, as is the external urethral sphincter, to retain urine within the bladder. This state is typically accompanied by urinary urgency due to the increased volume of urine.
On the right side, the diagram depicts the bladder during the process of micturition (urination). The red arrows pointing downwards indicate that the muscular wall of the bladder is contracting to expel urine. In this state, the internal sphincter muscles are relaxed, allowing urine to pass into the urethra. The external urethral sphincter also relaxes (not explicitly shown by an arrow but indicated by the text), which allows urine to flow out of the body through the urethra, shown by the yellow arrow.
This demonstrates the coordinated activity of the bladder and sphincter muscles in the process of urine storage and release. The bladder stores urine until a certain volume is reached, triggering a sensation of fullness and the need to urinate. During urination, the muscles of the bladder wall contract to push urine out, while the sphincters relax to allow the passage of urine.
Male Urinary Bladder:
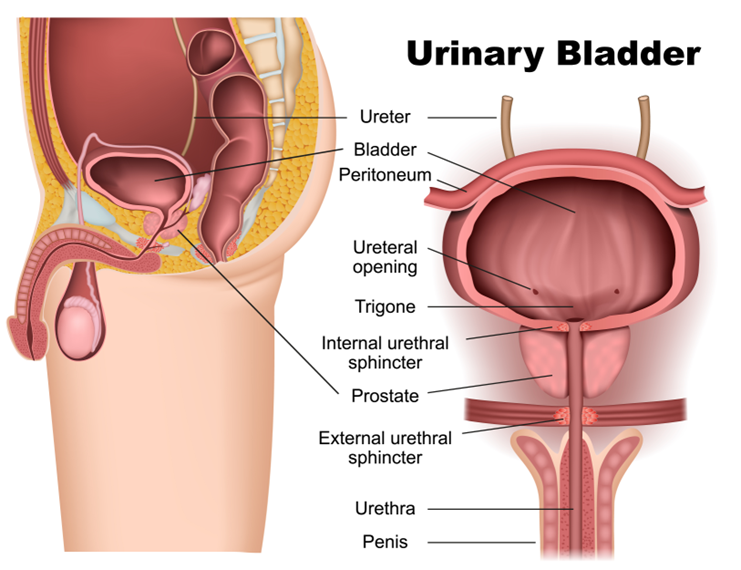
The image provides a detailed anatomical representation of the male urinary system, with a focus on the urinary bladder and its associated structures.
On the left side of the image, we see a cross-sectional view of the lower abdominal area, including the urinary bladder with its surrounding tissues and organs. The bladder is shown nestled within the pelvis, just above and behind the pubic bone. The ureters, which are tubes coming from the kidneys, are visible leading into the bladder, where they transport urine for storage.
The bladder is covered by a layer of tissue known as the peritoneum, which is part of the lining of the abdominal cavity. The ureteral openings are where the ureters connect to the bladder, and the trigone is a triangular area of the bladder wall between these openings and the urethral outlet. This area is clinically significant because infections tend to persist here.
On the right side of the image, we have a frontal view of the bladder and its outlet structures. The internal urethral sphincter is shown just below the bladder at the start of the urethra. This sphincter is an involuntary muscle that controls the flow of urine out of the bladder.
The prostate gland is situated below the internal sphincter and encircles the urethra. This gland is part of the male reproductive system and contributes fluid to semen during ejaculation.
Further down, the external urethral sphincter is shown, which is a voluntary muscle that allows for conscious control over the initiation of urination. Below this, the urethra extends through the penis, which is the organ through which urine exits the body.
The illustration serves to educate about the anatomy of the male urinary system, highlighting the path that urine takes from the kidneys to the external environment and the role of various structures in the storage and controlled release of urine.
Urine Formation Video 1 (38 secs):
Each kidney includes over a million blood filtering units called nephrons. Blood enters the nephron through a capillary bed called a glomerulus. It is surrounded by a cup-like structure, the glomerular capsule, which is the beginning of the duct called the renal tubule.
As blood flows through the glomerulus, blood pressure forces it against a specialized layer of cells that surrounds the capillaries. The layer of cells blocks blood cells and proteins, but lets waste and water pass through the glomerulus and into the glomerular capsule. The filtrate then flows into the proximal convoluted tubule. This process is called glomerular filtration. It is the first step in urine formation.
More Details:
Each kidney contains over a million nephrons, which are the basic structural and functional units responsible for filtering blood and forming urine. Understanding the structure and function of a nephron is key to comprehending how the kidneys maintain the body’s internal environment. Let’s delve into the details of the nephron and the process of glomerular filtration:
Structure of a Nephron
- Glomerulus: This is a network of tiny blood vessels (capillaries) where the filtration of blood begins. It’s here that blood enters the nephron.
- Glomerular (Bowman’s) Capsule: Surrounding the glomerulus is a cup-like structure known as the glomerular capsule. It collects the filtrate that is filtered out from the blood in the glomerulus.
- Renal Tubule: Extending from the glomerular capsule is a long, coiled structure called the renal tubule. The renal tubule is divided into several parts: the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule, which eventually connects to the collecting duct.
Glomerular Filtration Process
- Blood Entry: Blood enters each nephron through the afferent arteriole and flows into the glomerulus.
- Filtration Barrier: The glomerulus is surrounded by a specialized layer of cells, including podocytes, which form part of the filtration barrier. This barrier is selectively permeable.
- Filtration Process: As blood flows through the glomerulus, blood pressure forces water and small solutes (like ions, glucose, amino acids, and waste products) through the filtration barrier. Large molecules such as proteins and blood cells are too big to pass through this barrier and thus remain in the bloodstream.
- Collection of Filtrate: The filtrate, which includes water and these small solutes, enters the glomerular capsule and marks the beginning of the urinary filtrate.
- Flow into Renal Tubule: From the glomerular capsule, the filtrate flows into the proximal convoluted tubule, where the next stage of urine formation (reabsorption and secretion) takes place.
Significance of Glomerular Filtration
- First Step in Urine Formation: Glomerular filtration is the initial phase in the process of urine formation. It’s responsible for separating the filtrate from the blood.
- Regulation of Filtrate Composition: The filtration barrier is crucial in determining what becomes part of the filtrate and what stays in the blood, thus influencing the composition of the filtrate.
- Homeostasis: This process is essential for maintaining homeostasis in the body, including fluid balance, electrolyte balance, and waste removal.
The nephrons and the process of glomerular filtration highlight the complex and efficient ways in which the kidneys perform the critical function of filtering blood and maintaining the body’s internal balance. Understanding these processes is vital for grasping how various kidney diseases and disorders arise and how they can be managed or treated.
Urine Formation Video 2 (41 secs):
Glomerular filtration produces a plasma-like filtrate containing waste, but also water and other substances the body needs. As the filtrate passes out of the glomerular capsule and through the renal tubule, substances like water, essential ions, glucose, amino acids, and proteins are reabsorbed into the body through cells along the tube wall. At the same time, additional waste ions and hydrogen ions still in the blood pass from capillaries into the renal tubule. This process is called secretion. This process of reabsorbing water and nutrients and secreting additional waste creates urine. The urine passes out of the kidney, through the renal pelvis and ureters, and into the bladder.
More Details:
The process you’re describing is an essential part of how the kidneys filter blood and produce urine, a crucial function for maintaining the body’s internal balance. This involves several steps: glomerular filtration, tubular reabsorption, tubular secretion, and the excretion of urine. Let’s explore these in more detail:
Glomerular Filtration
- Location: This process occurs in the glomeruli, which are tiny clusters of blood vessels (capillaries) in the kidneys.
- Function: Blood pressure forces water and solutes (like waste products, glucose, amino acids, and ions) out of the blood and into the glomerular capsule, forming a plasma-like filtrate. This filtrate is free of larger proteins and cells, which are too big to pass through the glomerular filter.
Tubular Reabsorption
- Location: As the filtrate moves through the convoluted tubules of the nephron (the functional unit of the kidney), reabsorption occurs.
- Function: Essential substances in the filtrate, such as water, glucose, amino acids, and ions (like sodium and potassium), are reabsorbed into the bloodstream. This reabsorption is a selective process, ensuring that vital substances are conserved and not lost in urine.
- Mechanism: This process involves both passive and active transport mechanisms. For instance, water is often reabsorbed passively via osmosis, while glucose and amino acids are typically reabsorbed actively against their concentration gradient.
Tubular Secretion
- Location: Concurrently, in the renal tubule and the collecting duct.
- Function: This process involves the active transport of substances from the blood into the tubular fluid. It helps in the elimination of waste products (like urea and creatinine), excess ions, and drugs.
- Regulation: Secretion also plays a role in regulating the pH of the blood by secreting hydrogen ions and reabsorbing bicarbonate.
Formation of Urine
- The combined processes of filtration, reabsorption, and secretion lead to the formation of urine. This fluid contains waste products and unneeded substances in a concentrated form.
- Pathway: The urine flows from the nephrons to the renal pelvis, then travels down the ureters to the bladder, where it is stored until excretion through the urethra.
Physiological Importance
- Waste Elimination: Kidneys remove metabolic waste products and excess substances from the bloodstream.
- Regulation of Blood Volume and Pressure: By controlling the amount of water reabsorbed, the kidneys regulate blood volume and, consequently, blood pressure.
- Electrolyte Balance: The selective reabsorption and secretion of ions help maintain the electrolyte balance in the body.
- pH Balance: The secretion of hydrogen ions and reabsorption of bicarbonate are crucial for maintaining the acid-base balance in the body.
Overall, this complex process of filtration, reabsorption, secretion, and excretion by the kidneys is vital for the maintenance of homeostasis in the body, highlighting the kidneys’ crucial role in overall health.
Endocrine Gland Function Video (40 secs):
The endocrine system is composed of glands that regulate body functions, like the body’s reaction to the environment, the level of substances in the blood, metabolism and growth, immune responses, and sexual development and function. Each gland secretes chemical messengers called hormones directly into the bloodstream. Hormones dissolve into blood plasma and travel to specific body regions where they pass through the blood vessel walls and bind to targeted cells. It is by altering the function of individual cells that these hormones can influence the activity of the body’s individual tissues and organs.
More Details:
The endocrine system, a network of glands and the hormones they produce, plays a pivotal role in maintaining homeostasis within the body. This system intricately regulates a variety of critical bodily functions through a delicate and precise balance of hormone secretion and interaction.
Composition of the Endocrine System
- Glands and Hormones: The system consists of several glands, each producing specific hormones. Major endocrine glands include:
- Pituitary Gland: Often termed the “master gland,” it controls other endocrine glands and regulates growth and fluid balance.
- Thyroid Gland: Regulates metabolism, energy generation, and growth.
- Parathyroid Glands: Essential for calcium balance in the blood.
- Adrenal Glands: Produce cortisol and adrenaline, which regulate stress responses.
- Pancreas: Produces insulin and glucagon, vital for glucose metabolism.
- Gonads (Ovaries and Testes): Produce sex hormones essential for reproductive functions and sexual characteristics.
- Hormones: These are chemical substances that act as messengers. They are released into the bloodstream and exert their effects on distant organs or tissues.
Mechanism of Hormone Action
- Transportation: Hormones are typically dissolved in blood plasma and travel through the circulatory system to reach their target sites.
- Target Cells: Each hormone is designed to affect only specific cells or tissues, known as target cells. These cells have unique receptors that are compatible with a particular hormone.
- Cellular Interaction: Upon reaching the target cells, hormones bind to either surface receptors or intracellular receptors, depending on their nature (lipid-soluble or water-soluble). This binding initiates a cascade of cellular reactions.
- Physiological Effects: The interaction of hormones with their receptors can lead to a variety of outcomes, such as altering gene expression, modifying enzymatic activity, or changing the permeability of the cell membrane.
Regulatory Functions
- Metabolism and Homeostasis: Hormones like thyroid hormones and insulin play crucial roles in regulating metabolism and ensuring the balance of nutrients and energy in the body.
- Growth and Development: Growth hormone and sex hormones are vital for normal growth, development, and maturation.
- Stress Response: Hormones such as cortisol and adrenaline are key in managing the body’s response to stress.
- Reproductive Functions: Hormones regulate sexual development, reproductive cycles, fertility, and pregnancy.
- Immune Regulation: Certain hormones have roles in modulating immune responses and inflammatory processes.
Feedback Mechanisms
- The endocrine system is characterized by complex feedback mechanisms that regulate hormone levels. These mechanisms can be:
- Negative Feedback: Most common, where an increase in a specific hormone leads to actions that decrease its secretion, maintaining balance.
- Positive Feedback: Less common, where the release of a hormone leads to actions that stimulate further secretion of that hormone.
Understanding the endocrine system’s complexity is crucial for diagnosing and treating disorders related to hormonal imbalances, such as diabetes, thyroid disorders, and growth deficiencies. Advances in medical science continue to unravel the nuances of this system, offering deeper insights into its role in health and disease.
Endocrine System Hormones Video (42 secs):
Hormones travel through the bloodstream and come into contact with many cells. Each type of hormone affects only the behavior of specific targeted cells. A cell responds to a hormone only if it has receptors for that specific hormone. Some hormones bind to receptors on the surface of the target cell. Other hormones pass through the cell membrane and attach to receptors in the cytoplasm or nucleus. The binding of hormones to receptors on a cell triggers a cascade of actions within the cell that alters its physiological behavior. These changes affect many bodily functions including metabolism and growth, immune responses, and sexual development.
More Details:
Hormones are crucial chemical messengers in the body, playing an integral role in regulating a multitude of physiological processes. Their journey through the bloodstream is akin to a targeted delivery system, where they interact specifically with cells that are equipped to respond to them. This specificity is due to the presence of hormone receptors, which are specialized proteins either on the cell’s surface or within its interior.
Each hormone is designed to affect only certain cells, known as target cells. These are the only cells in the body that have receptors compatible with a specific hormone. The interaction between a hormone and its receptor is highly selective, similar to a lock and key mechanism. This specificity ensures that each hormone exerts its effects only on appropriate tissues and organs, thereby maintaining the body’s intricate balance.
Hormones can be broadly classified based on where their receptors are located:
- Surface Receptor Hormones: Some hormones, which are generally hydrophilic (water-loving), cannot pass through the lipid-rich cell membrane. These hormones bind to receptors located on the cell’s surface. An example of such hormones is insulin, which binds to surface receptors and regulates glucose uptake by cells.
- Intracellular Receptor Hormones: Other hormones, typically hydrophobic (fat-loving), can easily diffuse through the cell membrane. These hormones, like steroid hormones, bind to receptors located inside the cell, either in the cytoplasm or directly in the nucleus. For example, cortisol passes through the cell membrane and binds to intracellular receptors, affecting the transcription of specific genes.
Upon binding to its receptor, a hormone triggers a series of biochemical events inside the cell, often referred to as a signal transduction pathway. This cascade can vary greatly depending on the type of hormone and cell, but the general outcome is a change in the cell’s behavior. This may include:
- Altering Gene Expression: Hormones like steroid hormones can change which genes are expressed in the nucleus, affecting protein synthesis and thereby altering the cell’s structure and function.
- Modifying Enzymatic Activity: Some hormones activate or inhibit enzymes within the cell, which can rapidly change the cell’s metabolic pathways.
- Changing the Cell’s Permeability: Certain hormones affect the cell membrane’s permeability, influencing the transport of substances in and out of the cell.
These hormone-induced changes impact numerous bodily functions. For instance:
- Metabolism and Growth: Hormones like thyroid hormones and growth hormone play pivotal roles in metabolism, growth, and development.
- Immune Responses: Hormones can modulate the immune system, with certain steroids having anti-inflammatory effects.
- Sexual Development and Reproduction: Hormones such as estrogen, progesterone, and testosterone are key in regulating sexual development, reproductive cycles, and fertility.
Understanding the precise mechanisms of hormone action is vital for comprehending how various conditions, such as hormonal imbalances and endocrine disorders, arise and how they can be effectively treated.
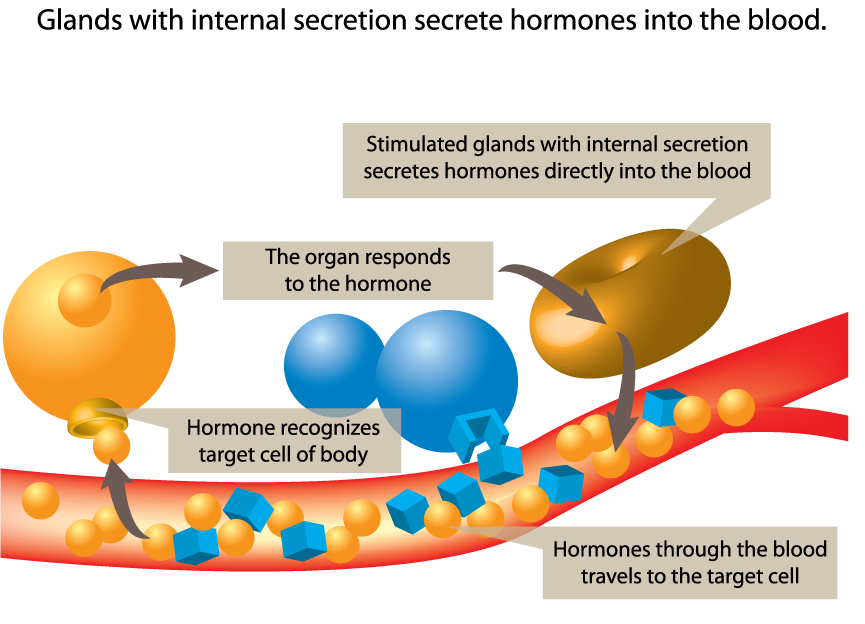
The image above is a schematic representation of the process by which glands with internal secretion, also known as endocrine glands, function in the human body. It’s designed to illustrate how hormones are released into the bloodstream and how they target specific organs or tissues. Here’s a breakdown of the depicted process:
- Glands with Internal Secretion: The image shows two glands, one of which is being stimulated. The stimulated gland is secreting hormones directly into the blood vessel, which is represented as a red and blue structure, symbolizing the flow of blood.
- Hormone Release and Travel: Small spherical and cubic shapes represent hormones, which are chemical messengers. These are shown being released from the stimulated gland and entering the bloodstream.
- Target Cell Recognition: The hormones travel through the blood vessel until they reach their target cells. The process of a hormone recognizing its target cell is depicted by a cubic hormone fitting into a corresponding cubic receptor on a cell, which represents the specificity of hormone action.
- Organ Response: Two large blue spheres represent the target organ, which responds to the hormone after recognition. The response could involve a change in the organ’s activity, such as increasing or decreasing the production of certain substances or altering its metabolic functions.
This diagram is key to understanding the endocrine system, emphasizing the specificity of hormone action. Each hormone has a particular target cell or organ that it influences, and this interaction is crucial for regulating a myriad of physiological processes, including growth, metabolism, and homeostasis. The process illustrated here underscores the significance of the hormonal communication network in maintaining the body’s internal environment.
Hormones Produced by the Ovaries:
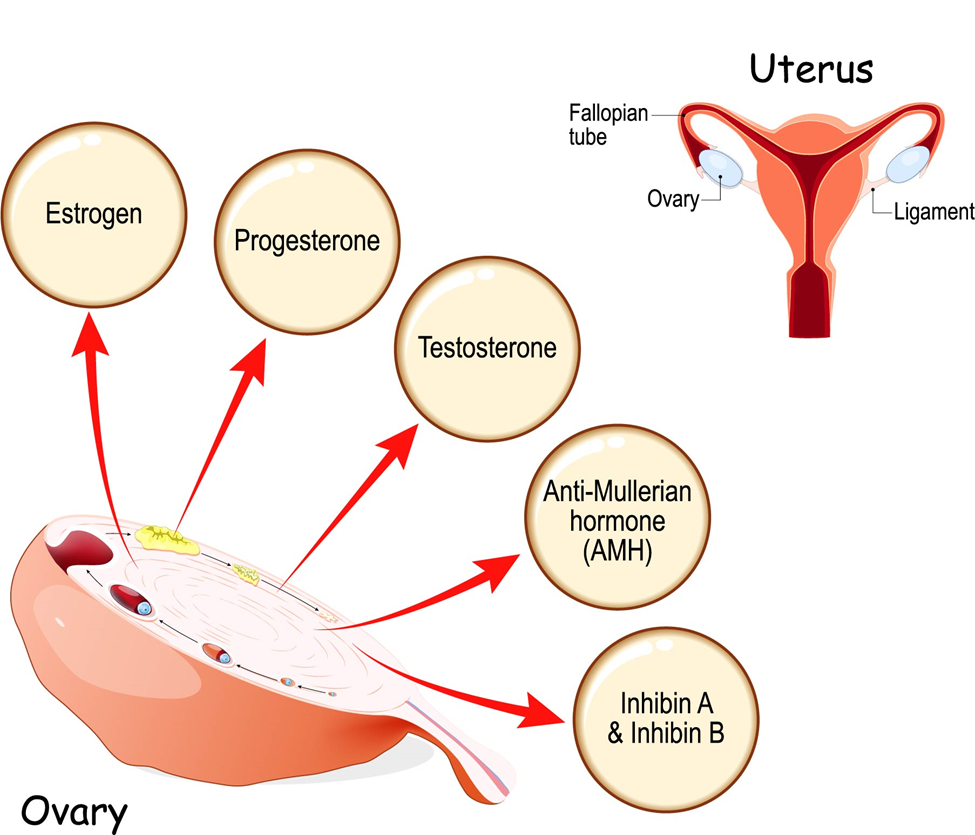
The image is an educational diagram that illustrates the various hormones produced by the ovaries and their relationship to the female reproductive system.
At the center of the image, there’s a detailed illustration of an ovary, a key reproductive organ in the female body. Arrows extend from the ovary to five circles, each representing a different hormone produced by ovarian tissue:
- Estrogen: Often considered one of the primary female sex hormones, it’s responsible for the development of female secondary sexual characteristics and the regulation of the menstrual cycle.
- Progesterone: This hormone plays a crucial role in the menstrual cycle and in maintaining the early stages of pregnancy.
- Testosterone: Commonly known as a male hormone, testosterone is also produced in smaller amounts by the ovaries. It’s important for bone strength and the development of lean muscle mass, among other functions.
- Anti-Müllerian Hormone (AMH): This hormone is involved in the development of sex organs and also serves as an indicator of a woman’s ovarian reserve.
- Inhibin A & Inhibin B: These hormones are involved in the regulation of the menstrual cycle, specifically in the control of FSH (follicle-stimulating hormone) production.
In the upper right corner of the diagram, a simplified representation of the female reproductive system is shown, including the uterus, fallopian tubes, and ligaments, with the ovaries in proximity. This visual connection emphasizes the role of the hormones in relation to the reproductive organs they influence.
The diagram encapsulates the complex endocrine functions of the ovaries and their integral role in female fertility, menstrual cycle regulation, and overall reproductive health. The selection and representation of these hormones underscore their significance in various physiological processes beyond reproduction, including bone health, muscle mass, and even the regulation of other hormones within the body.
Male Anatomy:
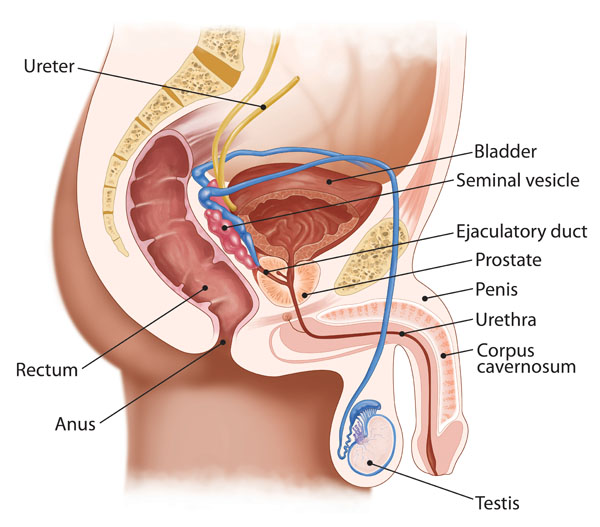
This is an anatomical illustration of the male pelvic region showing various structures of the urinary and reproductive systems.
- Ureter: The yellow tubes running from the top left to the bladder are the ureters. They transport urine from the kidneys to the bladder.
- Bladder: The bladder is shown as the brown organ at the top of the illustration. It collects and stores urine from the kidneys before it is voided through urination.
- Seminal Vesicle: Located just above the prostate, these paired structures are shown in blue. They secrete fluid that partly composes the semen.
- Ejaculatory Duct: The ejaculatory ducts are represented in blue, passing through the prostate. They transport sperm and seminal vesicle fluid to the urethra during ejaculation.
- Prostate: The prostate gland is indicated in red beneath the bladder. It secretes prostate fluid, one of the components of semen.
- Penis: The penis is depicted in profile with its internal structure. The urethra runs through it, allowing urine and semen to exit the body.
- Urethra: The urethra is the tube that carries urine from the bladder and semen from the reproductive tract outside of the body.
- Corpus Cavernosum: These are two cylindrical structures within the penis that fill with blood during an erection.
- Testis: The testis is represented at the bottom of the image, connected to the penis. It produces sperm and hormones like testosterone.
- Rectum: The rectum is the final section of the large intestine, terminating at the anus. It is not part of the urinary system but is an important structure in the pelvic area.
- Anus: The anus is the opening at the end of the digestive tract through which feces are expelled from the body.
The illustration provides an overview of how the male urinary and reproductive systems are arranged within the pelvic area, showing the close relationship between these two systems.
Male Reproductive System:
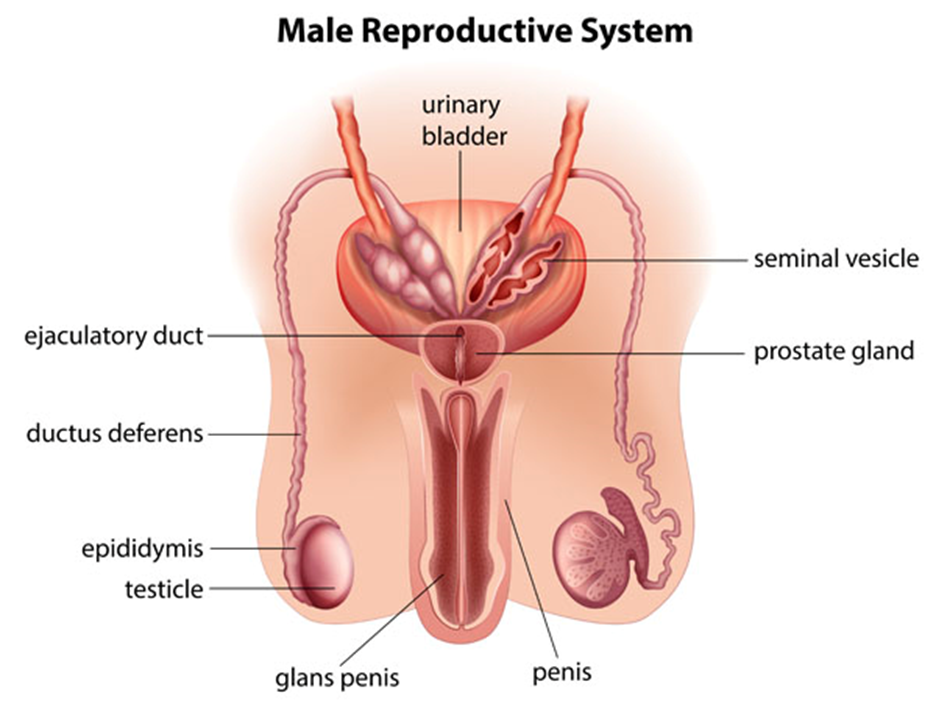
The image provides a detailed depiction of the male reproductive system along with related urinary structures.
- Urinary Bladder: Located at the top center, the bladder stores urine from the kidneys.
- Seminal Vesicle: Positioned above the prostate gland, these paired structures produce a fluid that forms part of the semen.
- Prostate Gland: Situated just below the bladder, surrounding the beginning of the urethra, the prostate contributes additional fluid to the semen.
- Ejaculatory Duct: These ducts run through the prostate gland and carry sperm and fluid from the seminal vesicles to the urethra.
- Ductus Deferens: Also known as the vas deferens, these tubes transport sperm from the epididymis in anticipation of ejaculation.
- Epididymis: The coiled structure on top of each testicle where sperm mature and are stored.
- Testicle: The oval organs (testes) located in the scrotum that produce sperm and hormones such as testosterone.
- Penis: The external organ used for urination and sexual intercourse.
- Glans Penis: The rounded head of the penis.
This illustration highlights the integral parts of the male reproductive system, explaining how they function together to produce, store, and transport sperm, as well as contribute to the formation of semen. The proximity of the reproductive system to the urinary bladder also shows the dual role of the penis in both excretory and reproductive functions.
Female Anatomy:
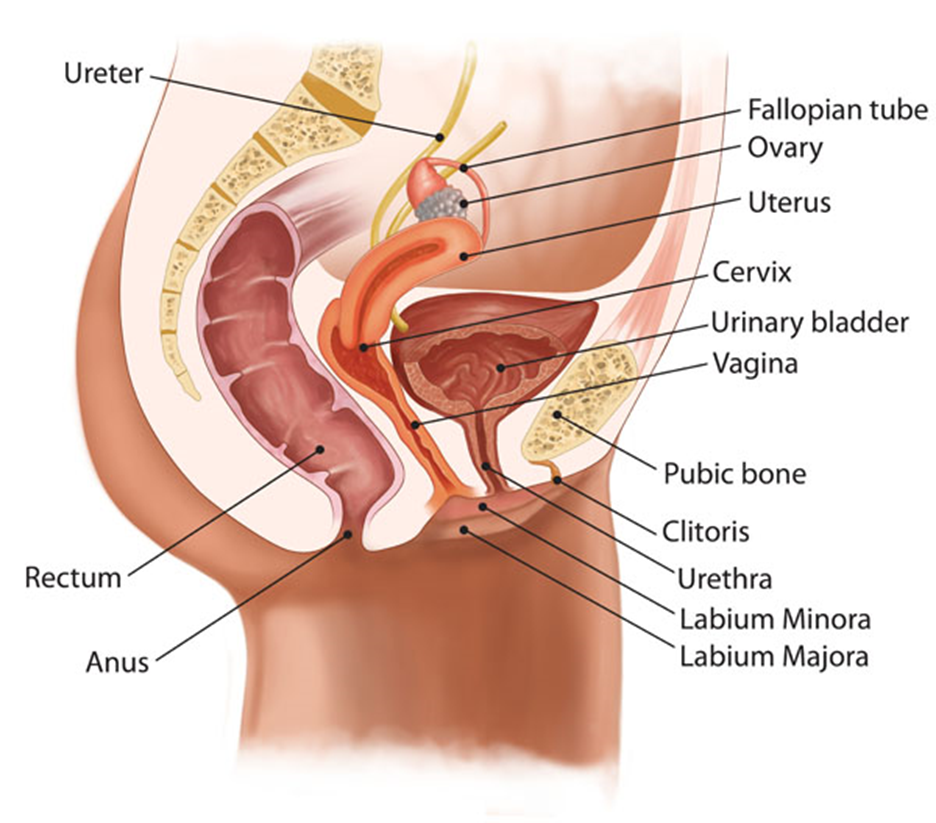
This image illustrates the female pelvic anatomy, showcasing both the urinary and reproductive systems.
- Ureter: These are the tubes that transport urine from the kidneys to the urinary bladder. They are shown entering the bladder from the top left.
- Fallopian Tube: A pair of tubes that carry eggs from the ovaries to the uterus.
- Ovary: The small, oval organs located on each side of the uterus, where eggs are produced.
- Uterus: The pear-shaped organ in the center, which is the site for fetal development during pregnancy.
- Cervix: The lower, narrow end of the uterus that opens into the vagina.
- Urinary Bladder: The muscular sac which stores urine from the kidneys, situated just above and in front of the vagina and cervix.
- Vagina: The muscular canal running from the cervix to the outside of the body, visible just below the bladder and cervix.
- Rectum: Located directly behind the vagina and cervix, it is the final section of the large intestine, ending at the anus.
- Anus: The opening at the end of the digestive tract from which feces are expelled.
- Pubic Bone: The lower front part of the pelvic bone, located at the bottom of the diagram.
- Clitoris: The small, sensitive, erectile part of the female genitals at the front of the vulva.
- Urethra: The tube that leads from the bladder to the external urinary opening, allowing urine to exit the body.
- Labium Minora: The smaller inner folds of the vulva.
- Labium Majora: The larger outer folds of the vulva.
The illustration is a comprehensive representation of the female pelvic region, demonstrating the proximity and arrangement of various urinary and reproductive structures within the pelvis.
Female Reproductive System:
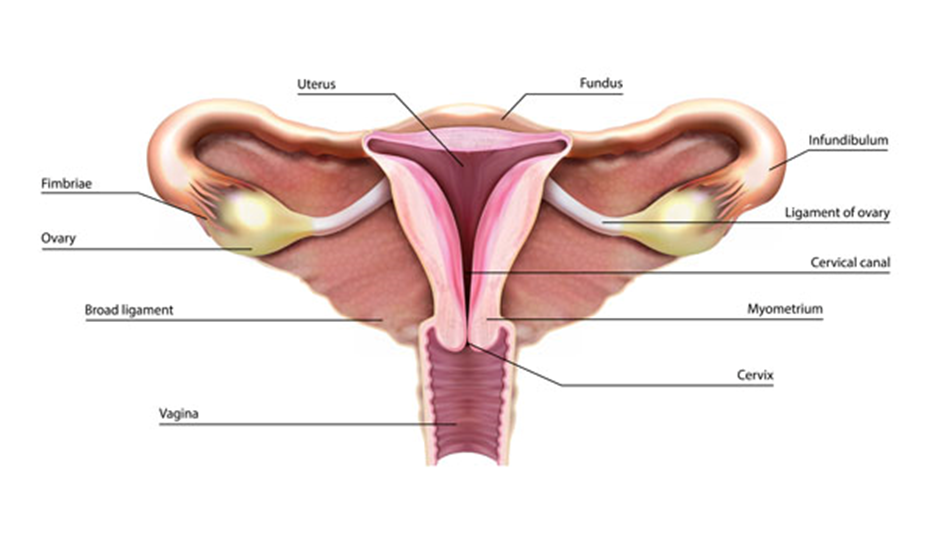
The image depicts the female reproductive system with its various components labeled, providing an internal view of the anatomical structure.
- Ovary: The almond-shaped structures on either side are the ovaries, which produce eggs (ova) and hormones like estrogen and progesterone.
- Fimbriae: The finger-like projections near each ovary help guide the released egg into the adjacent fallopian tube.
- Broad Ligament: This is a wide fold of peritoneum that connects the sides of the uterus to the walls and floor of the pelvis, providing support for the uterus and associated structures.
- Uterus: The large, central organ shaped somewhat like an inverted pear. It is the site where a fertilized egg implants and grows during pregnancy.
- Fundus: The rounded upper part of the uterus, which is above the openings of the fallopian tubes.
- Infundibulum: The funnel-shaped end of each fallopian tube near the ovary.
- Ligament of Ovary: These are the structures that anchor the ovaries to the uterus.
- Cervical Canal: The narrow passage through the cervix that connects the vagina to the internal part of the uterus.
- Myometrium: The thick, muscular layer of the uterus, which contracts during childbirth to help deliver the baby.
- Cervix: The lower part of the uterus that extends into the vagina. It acts as a gateway between the vagina and the uterus.
- Vagina: The muscular canal extending from the cervix to the exterior of the body. It receives the penis during sexual intercourse and serves as the birth canal.
This illustration is a concise educational tool for understanding the layout and function of the female reproductive organs, from the site of egg production to potential implantation and gestation.
