Tuning Fork Physics
Rossing, Thomas & Russell, Daniel & Brown, David. (1992). On the acoustics of tuning forks. American Journal of Physics. 60. 620-626. 10.1119/1.17116.
https://www.researchgate.net/publication/259017541_On_the_acoustics_of_tuning_forks
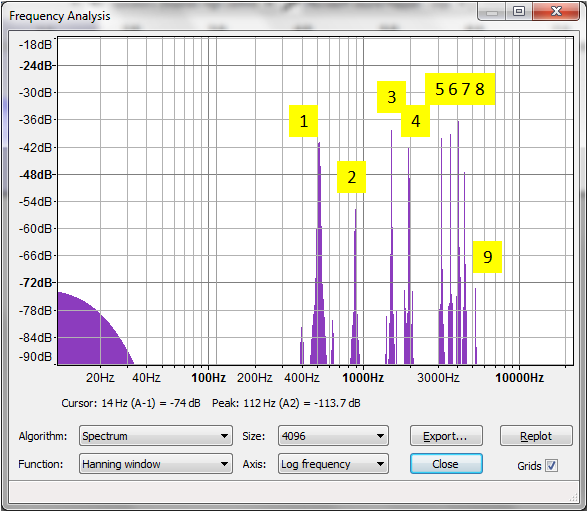
Tuning Fork Physics -- Part 1: sound waveform and spectral analysis
Tuning Fork Physics -- Part 2: modal analysis using FEA
Tuning Fork Physics -- Part 3: vibrations in super slow motion
Tuning Fork Physics -- Part 4: constrained and unconstrained vibrations
Predicting the tone of a tuning fork
https://sites.google.com/site/lucidanalysis/examples/tuningfork
Ultrasound Physics
ISBN 9780128015308, https://doi.org/10.1016/B978-0-12-801530-8.00005-0.
https://www.sciencedirect.com/science/article/pii/B9780128015308000050
RAMIREZ, ALEJANDRO; SCHWANE, JAMES A.; McFARLAND, CAROL; STARCHER, BARRY The effect of ultrasound on collagen synthesis and fibroblast proliferation in vitro, Medicine & Science in Sports & Exercise: March 1997 -- Volume 29 -- Issue 3 -- p 326-332
JACKSON, B. A., J. A. SCHWANE, and B. C STARCHER. Effect of ultrasound therapy on the repair of Achilles tendon injuries in rats. Med. Sci. Sports Exerc. Vol. 23, No. 2, pp. 171–176, 1991.
RUBIN D. Ultrasonic therapy: physiological basis and clinical application. California Medicine. 1958 Nov;89(5):349-351.
Bierman, W. Ultrasound in the treatment of scars. Arch. Phys. Med. Rehabil. 35: 209, 1954
Webster DF, Harvey W, Dyson M, Pond JB. The role of ultrasound-induced cavitation in the ‘in vitro’ stimulation of collagen synthesis in human fibroblasts. Ultrasonics. 1980 Jan;18(1):33-7. doi: 10.1016/0041-624x(80)90050-5. PMID: 7350723.
Kodama, Tetsuya & Tomita, Yukio & Watanabe, Yukiko & Koshiyama, Kenichiro & Yano, Takeru & Fujikawa, Shigeo. (2009). Cavitation Bubbles Mediated Molecular Delivery During Sonoporation. Journal of Biomechanical Science and Engineering. 4. 10.1299/jbse.4.124.
Koshiyama, Kenichiro & Kodama, Tetsuya & Yano, Takeru & Fujikawa, Shigeo. (2006). Molecular Dynamics Simulation of Water Pore Formation in Lipid Bilayer Induced by Shock Waves. The Journal of the Acoustical Society of America. 120. 583-587. 10.1063/1.2205541.
Vedadi, Mohammad & Choubey, Amit & Nomura, Ken-ichi & Kalia, R & Nakano, Aiichiro & Vashishta, P & van Duin, Adri. (2010). Structure and Dynamics of Shock-Induced Nanobubble Collapse in Water. Physical review letters. 105. 014503. 10.1103/PhysRevLett.105.014503.
Brujan, Emil & Vogel, Alfred & Blake, J.. (2002). The final stage of the collapse of a cavitation bubble close to a rigid boundary. Physics of Fluids. 14. 10.1063/1.1421102.
Interstitial Fluid and Lymphatic Drainage
Hopen S (August 27, 2022) Intrafasciomembranal Fluid Pressure: A Novel Approach to the Etiology of Myalgias. Cureus 14(8): e28475. doi:10.7759/cureus.28475 DOI: 10.7759/cureus.28475
Cenaj, O., Allison, D.H.R., Imam, R. et al. Evidence for continuity of interstitial spaces across tissue and organ boundaries in humans. Commun Biol 4, 436 (2021). https://doi.org/10.1038/s42003-021-01962-0
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7073453/
Reed RK, Rubin K. Transcapillary exchange: role and importance of the interstitial fluid pressure and the extracellular matrix. Cardiovasc Res. 2010 Jul 15;87(2):211-7. doi: 10.1093/cvr/cvq143. Epub 2010 May 13. PMID: 20472565.
Benias, P.C., Wells, R.G., Sackey-Aboagye, B. et al. Structure and Distribution of an Unrecognized Interstitium in Human Tissues. Sci Rep 8, 4947 (2018). https://doi.org/10.1038/s41598-018-23062-6
Abstract:
“The plasma volume is determined by fluid influx through drinking and outflux by renal excretion. Both fluxes are regulated according to plasma volume and composition through arterial pressure, osmoreceptors and vascular stretch receptors. As to the remaining part of the extracellular volume, the interstitial space, there is no evidence that its volume (IFV), pressure or composition are sensed in such a way as to influence water intake or excretion. Nevertheless, IFV is clearly regulated, often pari passu with the regulation of plasma volume. However, there are many exceptions to parallel changes of the two compartments, indicating the existence of automatic, local mechanisms guarding the net transfer of fluid between plasma and interstitium. Thus, a rise in arterial and/or venous pressure, tending to increase capillary pressure and net filtration, is counteracted by changes in the “Starling forces”: hydrostatic and colloid osmotic pressures of capillary blood and interstitial fluid. These “oedemapreventing mechanisms” (A. C. Guyton) may be listed as follows: Vascular mechanisms, modifying capillary pressure or interstitial fluid pressure (IFP). Increased transmural vascular pressure elicits precapillary constriction and thereby reduces the rise in capillary pressure. Counteracts formation of leg oedema in orthostasis. Venous expansion transmits pressure to the interstitium in encapsulated organs (brain, bone marrow, rat tail). Mechanisms secondary to increased net filtration, A rise in IFV will increase IFP, and thereby oppose further filtration. Favoured by lowcompliant interstitium. Reduction of interstitial COP through dilution and/or washout of interstitial proteins. A new steady state depends on increased lymph flow. Increased lymph flow permits a rise in net capillary filtration pressure. Low blood flow and high filtration fraction will increase local capillary COP.”
Aukland K. Distribution of body fluids: local mechanisms guarding interstitial fluid volume. Journal de Physiologie. 1984 ;79(6):395-400.
“Keep In mind that not only fibroblasts can produce collagens. Osteoblasts, chondroblasts, odontoblasts and smooth muscle cells can also synthesize collagens. Even epithelial cells can synthesize type IV collagen. You have already seen that the basement membrane contains type IV collagen in the basal lamina and type III collagen in the reticular lamina.” (pg 173)
Chapter 4: Connective Tissue. Cell Biology: Basic Tissues
Kierszenbaum, A. L., & Tres, L. L. (2020). Chapter 4: Connective Tissue. In Histology and cell biology: An introduction to pathology (5th ed., pp. 135-175). Philadelphia, PA: Elsevier.
Main sections include:
Arterioles Are the Stopcocks of the Circulation
Capillaries Permit the Exchange of Water, Solutes, and Gases
The Law of Laplace Explains How Capillaries Can Withstand High Intravascular
Pressures
The Endothelium Plays an Active Role in Regulating the Microcirculation
The Endothelium is at the Center of Flow-Initiated Mechanotransduction
The Endothelium Plays a Passive Role in Transcapillary Exchange
Diffusion Is the Most Important Means of Water and Solute Transfer Across the
Endothelium
Diffusion of Lipid-Insoluble Molecules Is Restricted to the Pores
Lipid-Soluble Molecules Pass Directly Through the Lipid Membranes of the
Endothelium and the Pores
Capillary Filtration Is Regulated by the Hydrostatic and Osmotic Forces Across the
Endothelium
Hydrostatic Forces
Hydrostatic Pressure Is the Principal Force in Capillary Filtration
Osmotic Forces
Balance of Hydrostatic and Osmotic Forces
The Capillary Filtration Coefficient Provides a Method to Estimate the Rate of Fluid
Movement Across the Endothelium
Disturbances in Hydrostatic–Osmotic Balance
Hypoxia-inducing factor(s) and angiogenesis
Pinocytosis Enables Large Molecules to Cross the Endothelium
Pappano, A. J., & Wier, W. G. (2019). Chapt. 8: Microcirculation and Lymphatics. In Cardiovascular physiology (pp. 139-154). Philadelphia, PA: Elsevier.
“progressive interstitial fibrosis” which is recognized as a key indicator of lymphedema, and edema in high protein content where there is a fibrous proliferation (adhesions).
The same book goes on to prove several of our theories about the work we do in the superficial adipose layer just underneath the skin. “In the fraction of patients (30–50%) who go on to develop clinically measurable lymphedema, sustained interstitial fluid stasis and ongoing chronic inflammation lead to extracellular matrix collagen deposition with resultant obliteration of capillary lymphatics and smooth muscle cell proliferation around collecting lymphatics” (pg 523).
“Interstitial fluid accumulates primarily (60–70% of the total excess volume) in the subcutaneous tissues between adipose tissues and around small veins.”
“Progressive fibro-fatty deposition makes lymphedema therapy more resistant to compressive therapies.” and “Lymphedema may therefore simply be a fibrotic disorder with loss of functional parenchyma (i.e. capillary and collecting lymphatics) due to progressive fibrosis” (pg. 524).
Therefore, both free fluid pockets and fascia adhesions together create “compartmentalized fascia” or more specifically pressurized fluids compartmentalized within a boundary of fascia fibers. Normally within the adipose layers there is little pressure increase when more fluid is released by the arterial capillaries. The proteoglycan gel and fascia will respond to spread the new fluid volume across the gel-filled space. When something happens to that same space that allows the fluid to separate from the gel, we get pockets of free fluid that does create an increase in hydrostatic pressure.
Lymphatic Pathophysiology in Chapter 10 on Fibrosis
Sidawy, A., Perler, B. and Rutherford, R., 2019. Rutherford’s Vascular Surgery And Endovascular Therapy. 9th ed. United States: Philadelphia, PA : Elsevier, [2019].
“Although almost all the fluid in the interstitium normally is entrapped within the tissue gel, occasionally small rivulets of “free” fluid and small free fluid vesicles are also present, which means fluid that is free of the proteoglycan molecules and therefore can flow freely. When a dye is injected into the circulating blood, it often can be seen to flow through the interstitium in the small rivulets, usually coursing along the surfaces of collagen fibers or surfaces of cells.
The amount of “free” fluid present in normal tissues is slight—usually less than 1 percent. Conversely, when the tissues develop edema, these small pockets and rivulets of free fluid expand tremendously until one half or more of the edema fluid becomes freely flowing fluid independent of the proteoglycan filaments.”
The Microcirculation and Lymphatic System: Capillary Fluid Exchange, Interstitial Fluid, and Lymph Flow Chapter 16, 189-201
Khonsary SA. Guyton and Hall: Textbook of Medical Physiology. Surg Neurol Int. 2017;8:275. Published 2017 Nov 9. doi:10.4103/sni.sni_327_17
“The functions of the lymphatic circulation include:
- the prevention and resolution of edema;
- maintenance of interstitial fluid homeostasis,
- immune traffic (the regulated transit of antigen-presenting cells to the lymphoid organs),
- and lipid absorption from the gastrointestinal tract.
In order to accomplish these various, intricate physiological functions, the lymphatic system relies upon a complex anatomic configuration of vascular conduits that is under exquisite physiological control.
As a vasculature, healthy lymphatics provide a unidirectional, blind-ended conduit of fluid from the tissue interstitium to the central venous circulation. The initial lymphatics, the most afferent components of the lymphatic vasculature, are in direct contiguity with the intercellular matrix, where fluid gains entry into the lymphatic vasculature. The transition from interstitial matrix to lymphatic space is delineated by the presence of an endothelial lining in the latter; once the fluid gains entry into the lymphatic endothelial-lined cavity of the initial lymphatics, it can be termed ‘lymph’. These initial thin-walled lymphatics can be equivalently termed ‘lymphatic capillaries’ and have a caliber of 30–80 μm. Lymphatic capillaries lack a basement membrane and smooth muscle cells (SMC), solely relying on the elastic fibers of the extracellular matrix for initiation of lymph drainage to reach the precollecting and collecting vessels. The specialized LECs have a distinct oak-leaf shape adorned by unique button-like junctions that characterize these the interfaces among cells and comprise the flap-like portals of entry into the lymphatic capillary. Conformational changes based on fluid and pressure dynamics of the extracellular matrix facilitate the opening and closing of these junctions. These large potential openings facilitate the entry of immune cells and larger structures into the lymph. Pericytes are absent from these circulatory conduits. The endothelial cells of the initial lymphatics are attached to the collagen fibers of the extracellular matrix through specialized anchoring filaments (Figure 4.1). As a result of absent basement membranes and SMCs, they solely rely on the elastic fibers of the extracellular matrix for entry of fluid into the lymphatic lumen.” (pgs 24-25)
Reference: Anatomy and Vasculature of Lymphatics.pdf
Principles and Practice of Lymphedema Surgery by STANLEY G. ROCKSON
Chapter 4: Anatomy and Structural Physiology of the Lymphatic System
“Fluids are thus forced by tissue pressure into the lumen of lymph capillaries so that we have to do also in this case with a filtration through the capillary walls, true, a filtration in the opposite sense, i.e. one directed from the interstitial space into the capillaries. But these measurements are, to say the least, of a doubtful value. To begin with, it is rather obscure what in point of fact is “forced” into the lymph capillaries by the difference of pressure under normal conditions when there is no free fluid in the connective tissue. In cases, on the other hand, where the skin contained oedema fluid, McMaster found the average fluid pressure to be 0-5 cm lower than the “tissue resistance” which makes it extremely probable that — when free fluid is actually present as it is, for instance, in oedema or in the lumen of lymph capillaries — the method in question will yield lower values so that there seems to exist no difference of pressure between extra- and intracapillary fluids.
The situation is essentially different when free fluid is actually present in the connective tissue. It is known from McMaster’s experiments that the pressure of the interstitial fluid may have a fairly high value and reach even a level of 20 cm water. Differences between tissue pressure and intra-lymph capillary pressure can be quite significant and facilitate a “filtration” of the fluid into the lymphatics. We want, in any case, to make it clear that — in our opinion — a tissue pressure higher than intralymphatic pressure cannot constitute the sole and decisive factor responsible for the absorption through lymphatic capillaries. Zhdanov (1952), for instance, emphasises in his monograph on the lymph vascular system that the physiological and anatomical properties of the lymph capillaries, the fact that their permeability exceeds that of the blood vessels, a direct connection with the ground substance of the connective tissue, the possibility of strong fluctuations of calibre and the physiological activity of the lymph capillary endothelium are surely important factors of the absorption into the lymph capillaries.
It must be admitted, however, that the problem of the passage of fluid, dissolved molecules and corpuscular elements from the blood into the lumen of the lymphatic capillaries is, in many respects, far from being solved.
Langen (1963) felt therefore, that the existing concepts regarding lymph formation failed to explain the observed facts and he was tempted to propose another solution. He surmised the presence of structures exerting a valve-like function and, permitting the extravasation of plasma proteins and even of blood corpuscles in the endothelial cells of blood capillaries. Some kind of a channel formed by the extrusion of the capillary basal membrane would then ensure a direct communication of the capillaries with the junction of the lymphatic vessels; the material which has passed between the two layers of the blood capillary wall is carried along this channel to the lymphatic system. At present no evidence exists to corroborate this interesting theory.” (Chapter 8, pgs 418-419)
“The results discussed in the foregoing paragraphs make it obvious that the permeability of connective tissues, the diffusion of water and dissolved substances, should not be regarded as a merely passive process. Although spreading in the connective tissues betrays a close similarity to phenomena observable in vitro in different colloidal systems, it has been shown that diverse physiological and pharmacological agents may cause profound alterations in the permeability of connective tissues. Such alterations are obviously of enzymatic origin (e.g. hyaluronidase effect) or provoked by a change in the structure of the ground substance. This consideration induced us to study the effect of metabolic and enzyme poisons on permeability.” (pg 404)
Citation Book: Rusznyák, István. Lymphatics and Lymph Circulation. Elsevier Science. Kindle Edition.
“Two mechanisms protecting against edema (i.e., edema safety factors) are evident from Figure 3.2, assuming that interstitial pressure is normally negative: 1) Since interstitial pressure must rise above 2 cmH2O for lymph flow to plateau, large changes in interstitial pressure can be accommodated before edema develops, and 2) An elevated lymph flow will quickly return the interstitial volume back to normal levels, as long as the excess volume does not exceed the capacity of the lymphatic circulation. Thus, a small increase in interstitial volume greatly increases its pressure, promoting lymph flow that acts to restore the interstitial volume to normal.”
Scallan J, Huxley VH, Korthuis RJ. Capillary Fluid Exchange: Regulation, Functions, and Pathology. San Rafael (CA): Morgan & Claypool Life Sciences; 2010. Chapter 3, The Lymphatic Vasculature. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53448/
Bradbury MW, Westrop RJ. Factors influencing exit of substances from cerebrospinal fluid into deep cervical lymph of the rabbit. J Physiol. 1983;339:519-534. doi:10.1113/jphysiol.1983.sp014731
Bradbury MW, Cole DF. The role of the lymphatic system in drainage of cerebrospinal fluid and aqueous humour. J Physiol. 1980;299:353-365. doi:10.1113/jphysiol.1980.sp013129
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1279229/
Ikomi, F, Hiruma, S. Relationship between shape of peripheral initial lymphatics and efficiency of mechanical stimulation–induced lymph formation. Microcirculation. 2020; 27:e12606. https://doi.org/10.1111/micc.12606
Sleboda DA, Roberts TJ. Internal fluid pressure influences muscle contractile force. Proc Natl Acad Sci U S A. 2020;117(3):1772-1778. doi:10.1073/pnas.1914433117
Qiuyun Wang, Shaopeng Pei, X. Lucas Lu, Liyun Wang, Qianhong Wu,
On the characterization of interstitial fluid flow in the skeletal muscle endomysium,
Journal of the Mechanical Behavior of Biomedical Materials, Volume 102, 2020,
103504, ISSN 1751-6161,
https://doi.org/10.1016/j.jmbbm.2019.103504
Evertz LQ, Greising SM, Morrow DA, Sieck GC, Kaufman KR. Analysis of fluid movement in skeletal muscle using fluorescent microspheres. Muscle Nerve. 2016;54(3):444-450. doi:10.1002/mus.25063
TRZEWIK, J., MALLIPATTU, S.K., ARTMANN, G.M., DELANO, F.A. and SCHMID-SCHONBEIN, G.W. (2001), Evidence for a second valve system in lymphatics: endothelial microvalves. FASEB J, 15: 1711-1717. https://doi.org/10.1096/fj.01-0067com
Stewart RH. A Modern View of the Interstitial Space in Health and Disease. Front Vet Sci. 2020;7:609583. Published 2020 Nov 5. doi:10.3389/fvets.2020.609583
Dongaonkar RM, Laine GA, Stewart RH, Quick CM. Balance point characterization of interstitial fluid volume regulation. Am J Physiol Regul Integr Comp Physiol. 2009;297(1):R6-R16. doi:10.1152/ajpregu.00097.2009
Kodama, Tetsuya & Tomita, Y.. (2000). Cavitation bubble behavior and bubble-shock wave interaction near a gelatin surface as a study of vivo bubble dynamics. Applied Physics B: Lasers and Optics. 70. 139-149. 10.1007/s003400050022.
Brujan, Emil & Vogel, Alfred & Blake, J.. (2002). The final stage of the collapse of a cavitation bubble close to a rigid boundary. Physics of Fluids. 14. 10.1063/1.1421102.
Kodama, Tetsuya & Tomita, Yukio & Watanabe, Yukiko & Koshiyama, Kenichiro & Yano, Takeru & Fujikawa, Shigeo. (2009). Cavitation Bubbles Mediated Molecular Delivery During Sonoporation. Journal of Biomechanical Science and Engineering. 4. 10.1299/jbse.4.124.
“Ultrasound has emerged as a promising means to effect controlled delivery of therapeutic agents through cell membranes. One possible mechanism that explains the enhanced permeability of lipid bilayers is the fast contraction of cavitation bubbles produced on the membrane surface, thereby generating large impulses, which, in turn, enhance the permeability of the bilayer to small molecules”
Fu, Haohao & Comer, Jeffrey & Cai, Wensheng & Chipot, Chris. (2015). Sonoporation at Small and Large Length Scales: Effect of Cavitation Bubble Collapse on Membranes. The Journal of Physical Chemistry Letters. 6. 413-418. 10.1021/jz502513w.
Krasovitski, Boris & Frenkel, Victor & Shoham, Shy & Kimmel, Eitan. (2011). Intramembrane cavitation as a unifying mechanism for ultrasound-induced bioeffects. Proceedings of the National Academy of Sciences of the United States of America. 108. 3258-63. 10.1073/pnas.1015771108.
Focal, Local, and Percussion Vibration
Germann D, El Bouse A, Shnier J, Abdelkader N, Kazemi M. Effects of local vibration therapy on various performance parameters: a narrative literature review. J Can Chiropr Assoc. 2018 Dec;62(3):170-181. PMID: 30662072; PMCID: PMC6319432.
Konrad A, Glashüttner C, Reiner MM, Bernsteiner D, Tilp M. The Acute Effects of a Percussive Massage Treatment with a Hypervolt Device on Plantar Flexor Muscles’ Range of Motion and Performance. J Sports Sci Med. 2020 Nov 19;19(4):690-694. PMID: 33239942; PMCID: PMC7675623.
Škarabot, J., Mesquita, R.N.O. and Ansdell, P. (2019), Elucidating the neurophysiology of local vibration: changes in neuromodulatory drive rather than presynaptic inhibition?. J Physiol, 597: 5753-5755. https://doi.org/10.1113/JP279018
Souron, R., Baudry, S., Millet, G.Y. and Lapole, T. (2019), Vibration‐induced depression in spinal loop excitability revisited. J Physiol, 597: 5179-5193. https://doi.org/10.1113/JP278469
Desmedt, John E., Godaux, Emile, (1978), Mechanism of the vibration paradox: excitatory and inhibitory effects of tendon vibration on single soleus muscle motor units in man. The Journal of Physiology, 285 doi: 10.1113/jphysiol.1978.sp012567.
https://physoc.onlinelibrary.wiley.com/doi/10.1113/jphysiol.1978.sp012567
Roll, J.P., Vedel, J.P. & Ribot, E. Alteration of proprioceptive messages induced by tendon vibration in man: a microneurographic study. Exp Brain Res 76, 213–222 (1989). https://doi.org/10.1007/BF00253639
Free PDF:
Transducers used in this type of experiment:
Lundeberg TC. Vibratory stimulation for the alleviation of chronic pain. Acta Physiol Scand Suppl. 1983;523:1-51. PMID: 6609524.
Murillo N, Valls-Sole J, Vidal J, Opisso E, Medina J, Kumru H. Focal vibration in neurorehabilitation. Eur J Phys Rehabil Med. 2014 Apr;50(2):231-42. PMID: 24842220.
Saggini R, Bellomo RG. Integration to focal vibration in neurorehabilitation. Eur J Phys Rehabil Med. 2015 Aug;51(4):508. Epub 2014 Nov 11. PMID: 25384515.
Rosenkranz, K. and Rothwell, J.C. (2004), The effect of sensory input and attention on the sensorimotor organization of the hand area of the human motor cortex. The Journal of Physiology, 561: 307-320.
https://doi.org/10.1113/jphysiol.2004.069328
https://physoc.onlinelibrary.wiley.com/doi/epdf/10.1113/jphysiol.2004.069328
Burke, D, Hagbarth, K E, Löfstedt, L, Wallin, B G, (1976), The responses of human muscle spindle endings to vibration during isometric contraction.. The Journal of Physiology, 261 doi: 10.1113/jphysiol.1976.sp011581.
https://physoc.onlinelibrary.wiley.com/doi/epdf/10.1113/jphysiol.1976.sp011581
Abstract:
“Recent studies have suggested that vibration therapy may have a positive influence on motor symptoms in individuals with Parkinson’s disease (PD). However, quantitative evidence of these benefits is scarce, and the concept of “whole-body” vibration in these studies is vague. The objectives of the current study were to evaluate the influence of vibration on motor symptoms and functional measures in PD by delivering sound waves to the entire body. We delivered whole body sound wave vibration to 40 individuals with PD using a Physioacoustic Chair, a piece of equipment with speakers spaced throughout the chair permitting a series of programmed low frequency sound waves through the body. Using a parallel cross-over design we utilized the Unified Parkinson’s Disease Rating Scale (UPDRS), quantitative gait assessments, and a grooved pegboard for upper limb control. Improvements were seen in all symptom, motor control and functional outcome measures at the time of assessment. Specifically, a significant decrease in rigidity, and tremor were shown, as well as a significant increase in step length and improved speed on the grooved pegboard task. Results of this initial investigation provide support for vibration therapy as a non-pharmacological treatment alternative. Long-term benefits of vibration therapy will require further research.”
King, Lauren & Ahonen, Heidi. (2009). Short-term effects of vibration therapy on motor impairments in Parkinson’s disease. NeuroRehabilitation. 25. 297-306. 10.3233/NRE-2009-0528
Rossing, Thomas & Russell, Daniel & Brown, David. (1992). On the acoustics of tuning forks. American Journal of Physics. 60. 620-626. 10.1119/1.17116.
https://www.researchgate.net/publication/259017541_On_the_acoustics_of_tuning_forks
Shomoto K, Takatori K, Morishita S, Nagino K, Yamamoto W, Shimohira T, Shimada T. Effects of ultrasound therapy on calcificated tendinitis of the shoulder. J Jpn Phys Ther Assoc. 2002;5(1):7-11. doi: 10.1298/jjpta.5.7. PMID: 25792924; PMCID: PMC4316484.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316484/
Fascia and Fibroblasts
“In order for the wound-healing process to take place after an injury, the cells require, as previously mentioned, mechanical loading. When the tissue is immobilized after an injury, a disturbance of normal wound healing occurs, at least in the proliferation phase (Fig. 9.2 not shown here).
A further disturbance of wound healing could occur when the cells are not getting enough of the nutrients they need to build the matrix components. This could happen when the circulation in the tissue is not sufficient.”
Liem, Torsten; Tozzi, Paolo; Chila, Anthony. Fascia in the Osteopathic Field (Kindle Locations 2843-2845). Handspring Pub Ltd. Kindle Edition.
“When fasciae are not moved sufficiently for long periods of time, morphologic changes in the tissue, such as fibrosis, can develop. This situation can be compared with the late phase in Dupuytren’s contracture. The first changes occur in the matrix, especially in the ground substance.”
Liem, Torsten; Tozzi, Paolo; Chila, Anthony. Fascia in the Osteopathic Field (Kindle Locations 2910-2912). Handspring Pub Ltd. Kindle Edition.
“The structural organization of the subcutis and the mechanical behavior of the superficial fascia and retinacula cutis in the different regions of the body may also influence the modality of manual treatment of the superficial and deep fascia. It is evident that in areas with loose and thin retinacula cutis, superficial massage to the skin will be unlikely to affect the deep fascia (except for possible indirect effects). To mechanically affect the deep fascia the subcutaneous fatty tissue must be displaced, so it is necessary to use a small-surface localized contact and to point directly into the deeper planes.”
Citation Book: Liem, Torsten; Tozzi, Paolo; Chila, Anthony. Fascia in the Osteopathic Field (Kindle Locations 5002-5005). Handspring Pub Ltd. Kindle Edition.
“There is a particularly fascinating receptor known as an integrin. Integrins are adhesive in nature. They stick each cell to the ECM. What makes integrins unique is that they respond not to chemical stimuli but to mechanical stimuli. They are sensitive to both stretch and vibration. It is as if each cell in the body was plugged into the ECM so that it can also monitor the environment by listening to it.
When the integrin is stimulated, it responds by creating electrochemical changes at the cellular level. The process of creating changes via mechanical pressure and vibration at the cellular level is called mechanotransduction.”
(Pg 12 of 154)
“In the simplest possible terms, the ECM is involved in every process and function of the body. It also serves as the body’s intranet. The EDM makes sure all the cells are in communication with all the other cells, creating a body-wide signaling network (Oschman 2003, Langevin 2006) that transmits mechanical signals such as strain and vibration throughout the entire organism via the fascial web.” (Pg 12 of 154)
“Fascia responds according to mechanical supply and demand, and follows Wolff’s law. Fibroblasts are both spooling out more collagen where necessary and secreting collagenase, a collagen-eating enzyme, all based on signals of pressure and vibration, like a cellular public works department – building, knocking down, and cleaning up the collagen matrix.” (Pg 14 of 154)
“As a quick recap, the key player in mechanotransduction is integrin, which helps bind the cell to the extracellular matrix via the collagen matrix. When stimulated by pressure and vibration, integrin transmits that tension to the nucleus where chemical changes altering gene expressions, and even effecting which genes switch on and switch off, occur.” (Pg 33 of 154)
Book Citation: Lesondak, David. (2018). Fascia: What it is and Why it Matters. Handspring Pub Ltd. Kindle Edition.
Langevin, H.M. and Yandow, J.A. (2002), Relationship of acupuncture points and meridians to connective tissue planes. Anat. Rec., 269: 257-265. doi:10.1002/ar.10185
Yang C, Du YK, Wu JB, et al. Fascia and Primo Vascular System. Evid Based Complement Alternat Med. 2015;2015:303769. doi:10.1155/2015/303769
Findley TW. Fascia Research from a Clinician/Scientist’s Perspective. Int J Ther Massage Bodywork. 2011;4(4):1–6. doi:10.3822/ijtmb.v4i4.158
Gusmão CV, Belangero WD. HOW DO BONE CELLS SENSE MECHANICAL LOADING?. Rev Bras Ortop. 2015;44(4):299–305. Published 2015 Dec 8. doi:10.1016/S2255-4971(15)30157-9
Yu Bai, Lin Yuan, Kwang-Sup Soh, Byung-Cheon Lee, Yong Huang, Chun-lei Wang, Jun Wang, Jin-peng Wu, Jing-xing Dai, Janos Palhalmi, Ou Sha, David Tai Wai Yew, Possible Applications for Fascial Anatomy and Fasciaology in Traditional Chinese Medicine, Journal of Acupuncture and Meridian Studies, Vol 3, Issue 2, 2010, Pgs 125-132,
doi.org/10.1016/S2005-2901(10)60023-4.
http://www.sciencedirect.com/science/article/pii/S2005290110600234
Langevin H. M., Bouffard N. A., Fox J. R., et al. Fibroblast cytoskeletal remodeling contributes to connective tissue tension. Journal of Cellular Physiology. 2011;226(5):1166–1175. doi: 10.1002/jcp.22442.
Langevin H. M., Storch K. N., Snapp R. R., et al. Tissue stretch induces nuclear remodeling in connective tissue fibroblasts. Histochemistry and Cell Biology. 2010;133(4):405–415. doi: 10.1007/s00418-010-0680-3.
Abbott R. D., Koptiuch C., Iatridis J. C., Howe A. K., Badger G. J., Langevin H. M. Stress and matrix-responsive cytoskeletal remodeling in fibroblasts. Journal of Cellular Physiology. 2013;228(1):50–57. doi: 10.1002/jcp.24102
Bai Y., Wang J., Wu J.-P., et al. Review of evidence suggesting that the fascia network could be the anatomical basis for acupoints and meridians in the human body. Evidence-Based Complementary and Alternative Medicine. 2011;2011:6. doi: 10.1155/2011/260510.260510
Grinnell F. Fibroblast mechanics in three-dimensional collagen matrices. Journal of Bodywork and Movement Therapies. 2008;12(3):191–193.
Rhee S, Jiang H, Ho CH, Grinnell F. Microtubule function in fibroblast spreading is modulated according to the tension state of cell-matrix interactions. Proc Natl Acad Sci USA. 2007;104:5425–30.
Shoulders MD, Raines RT. Collagen structure and stability. Annu Rev Biochem. 2009;78:929–58.
Abbott RD, Koptiuch C, Iatridis JC, Howe AK, Badger GJ, Langevin HM. Stress and matrix-responsive cytoskeletal remodeling in fibroblasts. J Cell Physiol. 2013;228(1):50-57. doi:10.1002/jcp.24102
Brain and Body Physiology
Hladky SB, Barrand MA. Mechanisms of fluid movement into, through and out of the brain: evaluation of the evidence. Fluids Barriers CNS. 2014;11(1):26. Published 2014 Dec 2. doi:10.1186/2045-8118-11-26
Iliff JJ, Lee H, Yu M, Feng T, Logan J, Nedergaard M, Benveniste H. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest. 2013;123:1299–1309. doi: 10.1172/JCI67677.
Nedergaard M. Neuroscience. Garbage truck of the brain. Science. 2013;340:1529–1530. doi: 10.1126/science.1240514.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med. 2012;4:147ra111. doi: 10.1126/scitranslmed.3003748
ykova E, Nicholson C. Diffusion in brain extracellular space. Physiol Rev. 2008;88:1277–1340. doi: 10.1152/physrev.00027.2007
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2785730/
Brinker T, Stopa EG, Morrison J, Klinge PM. A new look at cerebrospinal fluid circulation. Fluids Barriers CNS. 2014;11:10. doi: 10.1186/2045-8118-11-10.
Nervous System
Birznieks I, McIntyre S, Nilsson HM, et al. Tactile sensory channels over-ruled by frequency decoding system that utilizes spike pattern regardless of receptor type. Elife. 2019;8:e46510. Published 2019 Aug 6. doi:10.7554/eLife.46510
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6684274/
Saal HP, Wang X, Bensmaia SJ. Importance of spike timing in touch: an analogy with hearing? Current Opinion in Neurobiology. 2016;40:142–149. doi: 10.1016/j.conb.2016.07.013.
Bove GM. Epi-perineurial anatomy, innervation, and axonal nociceptive mechanisms. Journal of Bodywork and Movement Therapies. 2008;12(3):185–190.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2610338/
LOEWENSTEIN WR, RATHKAMP R. The sites for mechano-electric conversion in a Pacinian corpuscle. J Gen Physiol. 1958;41(6):1245–1265. doi:10.1085/jgp.41.6.1245
Vallbo AB, Olausson H, Wessberg J, Kakuda N. Receptive field characteristics of tactile units with myelinated afferents in hairy skin of human subjects. The Journal of Physiology. 1995;483:783–795. doi: 10.1113/jphysiol.1995.sp020622
Saal HP, Delhaye BP, Rayhaun BC, Bensmaia SJ. Simulating tactile signals from the whole hand with millisecond precision. PNAS. 2017;114:E5693–E5702. doi: 10.1073/pnas.1704856114.
Town SM, Bizley JK. Neural and behavioral investigations into timbre perception. Front. Syst. Neurosci. 2013;7:88.
Strzalkowski ND, Incognito AV, Bent LR, Millar PJ. Cutaneous Mechanoreceptor Feedback from the Hand and Foot Can Modulate Muscle Sympathetic Nerve Activity. Front Neurosci. 2016;10:568. Published 2016 Dec 8. doi:10.3389/fnins.2016.00568
Zimmerman A., Bai L., Ginty D. D. (2014). The gentle touch receptors of mammalian skin. Science 346, 950–954. 10.1126/science.1254229
Yau J. M., Kim S. S., Thakur P. H., Bensmaia S. J. (2016). Feeling form: the neural basis of haptic shape perception. J. Neurophysiol. 115, 631–642. 10.1152/jn.00598.2015
Strzalkowski N. D., Triano J. J., Lam C. K., Templeton C. A., Bent L. R. (2015b). Thresholds of skin sensitivity are partially influenced by mechanical properties of the skin on the foot sole. Physiol. Rep. 3:e12425. 10.14814/phy2.12425
Strzalkowski N. D., Mildren R. L., Bent L. R. (2015a). Thresholds of cutaneous afferents related to perceptual threshold across the human foot sole. J. Neurophysiol. 114, 2144–2151. 10.1152/jn.00524.2015
Donadio V., Kallio M., Karlsson T. (2002a). Inhibition of human muscle sympathetic activity by sensory stimulation. J. Physiol. 544, 285–292. 10.1113/jphysiol.2002.019596
Cui J., Blaha C., Moradkhan R., Gray K. S., Sinoway L. I. (2006). Muscle sympathetic nerve activity responses to dynamic passive muscle stretch in humans. J. Physiol. 576, 625–634. 10.1113/jphysiol.2006.116640
Burke D., Hagbarth K. E., Löfstedt L., Wallin B. G. (1976). The responses of human muscle spindle endings to vibration of non-contracting muscles. J. Physiol. 261, 673–693. 10.1113/jphysiol.1976.sp011580
Burton A. R., Fazalbhoy A., Macefield V. G. (2016). Sympathetic responses to noxious stimulation of muscle and skin. Front. Neurol. 7:109. 10.3389/fneur.2016.00109
Bensmaia S. J., Hollins M. (2003). The vibrations of texture. Somatosens. Mot. Res. 20, 33–43. 10.1080/0899022031000083825
Beissner F., Meissner K., Bär K. J., Napadow V. (2013). The autonomic brain: an activation likelihood estimation meta-analysis for central processing of autonomic function. J. Neurosci. 33, 10503–10511. 10.1523/JNEUROSCI.1103-13.2013
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3685840/
Abraira V. E., Ginty D. D. (2013). The sensory neurons of touch. Neuron 79, 618–639. 10.1016/j.neuron.2013.07.051
Cauna N, Ross LL. The Fine Structure of Meissners Touch Corpuscles of Human Fingers. J Biophys Biochem Cy. 1960;8:467–482.
Hubbard SJ. A study of rapid mechanical events in a mechanoreceptor. The Journal of physiology. 1958;141:198–218.
Neural Synchronization
Benias, P.C., Wells, R.G., Sackey-Aboagye, B. et al. Structure and Distribution of an Unrecognized Interstitium in Human Tissues. Sci Rep 8, 4947 (2018). https://doi.org/10.1038/s41598-018-23062-6
Brette R. Computing with Neural Synchrony. PLoS Comput. Biol. 2012;8:e1002561.
ncbi.nlm.nih.gov/pmc/articles/PMC3375225/
Cedolin L, Delgutte B. Spatiotemporal representation of the pitch of harmonic complex tones in the auditory nerve. J. Neurosci. 2010;30:12712–12724.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2957107/
Mackevicius EL, Best MD, Saal HP, Bensmaia SJ. Millisecond Precision Spike Timing Shapes Tactile Perception. J. Neurosci. 2012;32:15309–15317.
Saal HP, Harvey MA, Bensmaia SJ. Rate and timing of cortical responses driven by separate sensory channels. Elife. 2015;4:7250–7257.
Cedolin L, Delgutte B. Pitch of complex tones: rate-place and interspike interval representations in the auditory nerve. J. Neurophysiol. 2005;94:347–362.
Accordion McKinney MF, Delgutte B. A possible neurophysiological basis of the octave enlargement effect. J Acoust Soc Am. 1999;73:1694–1700.
Muniak MA, Ray S, Hsiao SS, Dammann JF, Bensmaia SJ. The neural coding of stimulus intensity: linking the population response of mechanoreceptive afferents with psychophysical behavior. J. Neurosci. 2007;27:11687–11699.
Yau JM, Olenczak JB, Dammann JF, Bensmaia SJ. Temporal frequency channels are linked across audition and touch. Curr Biol. 2009;19:561–566.
Rauschecker JP, Tian B. Mechanisms and streams for processing of “what” and “where” in auditory cortex. Proc Natl Acad Sci U S A. 2000;97:11800–11806.
Fu KM, Johnston TA, Shah AS, Arnold L, Smiley J, Hackett TA, Garraghty PE, Schroeder CE. Auditory cortical neurons respond to somatosensory stimulation. Journal of Neuroscience. 2003;23:7510–7515.
Driver J, Noesselt T. Multisensory interplay reveals crossmodal influences on ‘sensory-specific’ brain regions, neural responses, and judgments. Neuron. 2008;57:11–23.
Salinas E, Hernandez A, Zainos A, Romo R. Periodicity and firing rate as candidate neural codes for the frequency of vibrotactile stimuli. J Neurosci. 2000;20:5503–5515.
aal HP, Vijayakumar S, Johansson RS. Information about complex fingertip parameters in individual human tactile afferent neurons. J Neurosci. 2009;29:8022–8031.
Pei YC, Hsiao SS, Bensmaia SJ. The tactile integration of local motion cues is analogous to its visual counterpart. Proc Natl Acad Sci U S A. 2008;105:8130–8135.
Johnson KO, Hsiao SS, Yoshioka T. Neural coding and the basic law of psychophysics. Neuroscientist. 2002;8:111–121.
Johansson RS, Vallbo AB. Tactile sensibility in the human hand: relative and absolute densities of four types of mechanoreceptive units in glabrous skin. J Physiol. 1979;286:283–300.
Jacobs AL, Fridman G, Douglas RM, Alam NM, Latham PE, Prusky GT, Nirenberg S. Ruling out and ruling in neural codes. Proc Natl Acad Sci U S A. 2009;106:5936–5941.
Gamzu E, Ahissar E. Importance of temporal cues for tactile spatial-frequency discrimination. J Neurosci. 2001;21:7416–7427.
Bensmaia SJ, Denchev PV, Dammann JF, 3rd, Craig JC, Hsiao SS. The representation of stimulus orientation in the early stages of somatosensory processing. J Neurosci. 2008;28:776–786.
Jóhannesson ÓI, Hoffmann R, Valgeirsdóttir VV, Unnþórsson R, Moldoveanu A, Kristjánsson Á. Relative vibrotactile spatial acuity of the torso. Exp Brain Res. 2017;235(11):3505–3515. doi:10.1007/s00221-017-5073-6
Circadian and Peripheral Rhythm
Roenneberg T, Merrow M. The Circadian Clock and Human Health. Curr Biol. 2016 May 23;26(10):R432-43. doi: 0.1016/j.cub.2016.04.011. Review.
Mohawk JA, Green CB, Takahashi JS. 2012. Central and peripheral circadian clocks in mammals. Annu. Rev. Neurosci. 35, 445–46210.1146/annurev-neuro-060909-153128
Lamia KA, Storch KF, Weitz CJ. Physiological significance of a peripheral tissue circadian clock. Proc Natl Acad Sci U S A. 2008;105:15172–15177.
Heyde I, Oster H. Differentiating external zeitgeber impact on peripheral circadian clock resetting. Sci Rep. 2019;9(1):20114. Published 2019 Dec 27. doi:10.1038/s41598-019-56323-z
Abraham U, Granada AE, Westermark PO, Heine M, Kramer A, Herzel H. Coupling governs entrainment range of circadian clocks. Mol. Syst. Biol. 2010;6:438.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3010105/
Granada AE, Cambras T, Diez-Noguera A, Herzel H. 2010. Circadian desynchronization. J. R. Soc. Interface Focus 1, 153–16610.1098/rsfs.2010.0002
Kevin D. Himberger, Hsiang-Yun Chien, Christopher J. Honey, Principles of Temporal Processing Across the Cortical Hierarchy, Neuroscience, Volume 389, 2018, Pages 161-174, ISSN 0306-4522, doi.org/10.1016/j.neuroscience.2018.04.030.
http://www.sciencedirect.com/science/article/pii/S0306452218302951
Zhang Y, Khorkova O, Rodriguez R, Golowasch J. Activity and neuromodulatory input contribute to the recovery of rhythmic output after decentralization in a central pattern generator. J Neurophysiol. 2009;101:372–386.
LeGates TA, Fernandez DC, Hattar S. Light as a central modulator of circadian rhythms, sleep and affect. Nat Rev Neurosci. 2014;15(7):443–454. doi:10.1038/nrn3743
Boivin DB. Influence of sleep-wake and circadian rhythm disturbances in psychiatric disorders. J Psychiatry Neurosci. 2000;25:446–58.
Kiessling S, Eichele G, Oster H. Adrenal glucocorticoids have a key role in circadian resynchronization in a mouse model of jet lag. J Clin Invest. 2010;120:2600–9.
Ruby NF, et al. Hippocampal-dependent learning requires a functional circadian system. Proc Natl Acad Sci U S A. 2008;105:15593–8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563080/
Karatsoreos IN, Bhagat S, Bloss EB, Morrison JH, McEwen BS. Disruption of circadian clocks has ramifications for metabolism, brain, and behavior. Proc Natl Acad Sci U S A. 2011;108:1657–62.
Balasubramaniam P, Jarina Banu L. Synchronization criteria of discrete-time complex networks with time-varying delays and parameter uncertainties. Cogn Neurodyn. 2014;8:199–215. doi: 10.1007/s11571-013-9272-y.
Qu J, Wang R, Yan C, Du Y (2013) Oscillations and synchrony in a cortical neural network. Cogn Neurodyn. doi:10.1007/s11571-013-9268-7
Shi X, Wang QY, Lu QS. Firing synchronization and temporal order in noisy neuronal networks. Cogn Neurodyn. 2008;2(3):195–206. doi: 10.1007/s11571-008-9055-z.
Sun WG, Wang RB, Wang WX, Cao JT. Analyzing inner and outer synchronization between two coupled discrete-time networks with time delays. Cogn Neurodyn. 2010;4(3):225–231. doi: 10.1007/s11571-010-9118-9.
Yu S, Huang DB, Singer W, et al. A small world of neuronal synchrony. Cereb Cortex. 2008;18(2):2891–2901. doi: 10.1093/cercor/bhn047.
Harris-Warrick RM. Neuromodulation and flexibility in central pattern generator networks. Curr Opin Neurobiol. 2011;21(5):685–692. doi: 10.1016/j.conb.2011.05.011.
Bartos M, Manor Y, Nadim F, Marder E & Nusbaum MP Coordination of fast and slow rhythmic neuronal circuits. J. Neurosci 19, 6650–6660 (1999).
Nadim F, Manor Y, Nusbaum MP & Marder E Frequency regulation of a slow rhythm by a fast periodic input. J. Neurosci 18, 5053–5067 (1998).
Lacquaniti F, Ivanenko YP, Zago M. Patterned control of human locomotion. J Physiol. 2012;590(10):2189–2199. doi: 10.1113/jphysiol.2011.215137.
Roenneberg T., Wirz-Justice A., Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms. 2003; 18: 80-90
https://www.cell.com/action/showPdf?pii=S0960-9822%2816%2930333-5
Damiola F, et al. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000;14:2950–2961. doi: 10.1101/gad.183500.
Erzberger A, Hampp G, Granada AE, Albrecht U, Herzel H. Genetic redundancy strengthens the circadian clock leading to a narrow entrainment range. J. R. Soc. Interface. 2013;10:20130221. doi: 10.1098/rsif.2013.0221.
Aton SJ, Herzog ED (2005) Come together, right.now: synchronization of rhythms in a mammalian circadian clock. Neuron 48: 531–534
Best JD, Maywood ES, Smith KL, Hastings MH (1999) Rapid resetting of the mammalian circadian clock. J Neurosci 19: 828–835
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6782190/
Gonze D, Bernard S, Waltermann C, Kramer A, Herzel H (2005) Spontaneous synchronization of coupled circadian oscillators. Biophys J 89: 120–129
Granada AE, Herzel H (2009) How to achieve fast entrainment? The timescale to synchronization. PLoS One 4: e7057.
Granados-Fuentes D, Prolo LM, Abraham U, Herzog ED (2004) The suprachiasmatic nucleus entrains, but does not sustain, circadian rhythmicity in the olfactory bulb. J Neurosci 24: 615–619
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6729269/
Roenneberg T, Dragovic Z, Merrow M (2005) Demasking biological oscillators: properties and principles of entrainment exemplified by the neurospora circadian clock. Proc Natl Acad Sci USA 102: 7742–7747
Westermark PO, Welsh DK, Okamura H, Herzel H (2009) Quantification of circadian rhythms in single cells. PLoS Comput Biol 5: e1000580.
Guo H, Brewer JM, Champhekar A, Harris RB, Bittman EL. Differential control of peripheral circadian rhythms by suprachiasmatic-dependent neural signals. Proc. Natl. Acad. Sci. USA. 2005;102:3111–3116.
Bordyugov G, Abraham U, Granada A, Rose P, Imkeller K, Kramer A, Herzel H. Physiology of Circadian Entrainment. J R Soc Interface. 2015 Jul 6;12(108):20150282. doi: 10.1098/rsif.2015.0282.
https://journals.physiology.org/doi/pdf/10.1152/physrev.00009.2009
Vibration, Oscillations, and Entrainment
Wilson CJ, Higgs MH, Simmons DV, Morales JC. Oscillations and Spike Entrainment. F1000Res. 2018 Dec 20;7. pii: F1000 Faculty Rev-1960. doi: 10.12688/f1000research.16451.1. eCollection 2018. Review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6305216/
Butcher PA, Taylor JA. Decomposition of a sensory prediction error signal for visuomotor adaptation. J Exp Psychol Hum Percept Perform. 2018 Feb;44(2):176-194. doi: 10.1037/xhp0000440. Epub 2017 May 15.
Schlerf JE, Ivry RB, Diedrichsen J. Encoding of Sensory Prediction Errors in the Human Cerebellum. Journal of Neuroscience. 2012;32(14):4913–4922.
Corbetta M, Patel G, Shulman GL. The reorienting system of the human brain: From environment to theory of mind. Neuron. 2008;58(3):306–324.
Logan RW, McClung CA. Rhythms of life: circadian disruption and brain disorders across the lifespan. Nat Rev Neurosci. 2019 Jan;20(1):49-65. doi: 10.1038/s41583-018-0088-y. Review.
Bordyugov G, Abraham U, Granada A, Rose P, Imkeller K, Kramer A, Herzel H. Tuning the phase of circadian entrainment. J R Soc Interface. 2015 Jul 6;12(108):20150282. doi: 10.1098/rsif.2015.0282.
Abraham U, Granada AE, Westermark PO, Heine M, Kramer A, Herzel H. 2010. Coupling governs entrainment range of circadian clocks. Mol. Syst. Biol. 6, 438 (10.1038/msb.2010.92)
Bernard S, Gonze D, Cajavec B, Herzel H, Kramer A (2007) Synchronization-induced rhythmicity of circadian oscillators in the suprachiasmatic nucleus. PLoS Comput Biol 3: e68.
Gonze D, Bernard S, Waltermann C, Kramer A, Herzel H (2005) Spontaneous synchronization of coupled circadian oscillators. Biophys J 89: 120–129
Granada AE, Herzel H (2009) How to achieve fast entrainment? The timescale to synchronization. PLoS One 4: e7057.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2745570/
Relógio A, Westermark PO, Wallach T, Schellenberg K, Kramer A, Herzel H. 2011. Tuning the mammalian circadian clock: robust synergy of two loops. PLoS Comp. Biol. 7, e1002309 (10.1371/journal.pcbi.1002309)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3240597/
Buhr ED, Yoo SH, Takahashi JS. 2010. Temperature as a universal resetting cue for mammalian circadian oscillators. Science 330, 379–385. (10.1126/science.1195262)
Rohling JH, Tjebbe vander Leest H, Michel S, Vansteensel MJ, Meijer JH. 2011. Phase resetting of the mammalian circadian clock relies on a rapid shift of a small population of pacemaker neurons. PLoS ONE 6, e25437 (10.1371/journal.pone.0025437)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3178639/
Škarabot, J., Mesquita, R.N.O. and Ansdell, P. (2019), Elucidating the neurophysiology of local vibration: changes in neuromodulatory drive rather than presynaptic inhibition?. J Physiol, 597: 5753-5755. https://doi.org/10.1113/JP279018
Souron, R., Baudry, S., Millet, G.Y. and Lapole, T. (2019), Vibration‐induced depression in spinal loop excitability revisited. J Physiol, 597: 5179-5193. https://doi.org/10.1113/JP278469
Desmedt, John E., Godaux, Emile, (1978), Mechanism of the vibration paradox: excitatory and inhibitory effects of tendon vibration on single soleus muscle motor units in man. The Journal of Physiology, 285 doi: 10.1113/jphysiol.1978.sp012567.
https://physoc.onlinelibrary.wiley.com/doi/10.1113/jphysiol.1978.sp012567
Roll, J.P., Vedel, J.P. & Ribot, E. Alteration of proprioceptive messages induced by tendon vibration in man: a microneurographic study. Exp Brain Res 76, 213–222 (1989). https://doi.org/10.1007/BF00253639
Free PDF:
Transducers used in this type of experiment:
Prediction Error & Cognitive Processing
Marko MK, Haith AM, Harran MD, Shadmehr R. Sensitivity to prediction error in reach adaptation. Journal of neurophysiology. 2012;108(6):1752–63.
Izawa J, Pekny SE, Marko MK, Haswell CC, Shadmehr R, Mostofsky SH. Motor learning relies on integrated sensory inputs in ADHD, but over-selectively on proprioception in autism spectrum conditions. Autism Res 5: 124–136, 2012b
Schlerf JE, Ivry RB, Diedrichsen J. Encoding of Sensory Prediction Errors in the Human Cerebellum. Journal of Neuroscience. 2012;32(14):4913–4922.
Popa LS, Ebner TJ. Cerebellum, Predictions and Errors. Front Cell Neurosci. 2019 Jan 15;12:524. doi: 10.3389/fncel.2018.00524. eCollection 2018.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6340992/
Barrett L. F., Simmons W. K. (2015). Interoceptive predictions in the brain. Nat. Rev. Neurosci. 16, 419–429. 10.1038/nrn3950
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4731102/
Chennu S, et al. Expectation and attention in hierarchical auditory prediction. J. Neurosci. 2013;33:11194–11205.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3718380/
Seth AK, Suzuki K, Critchley HD. An interoceptive predictive coding model of conscious presence. Front. Psychol. 2011;2:395.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3254200/
Feldman H, Friston KJ. Attention, uncertainty, and free-energy. Front. Hum. Neurosci. 2010;4:215.
Oosterwijk S, et al. States of mind: emotions, body feelings, and thoughts share distributed neural networks. Neuroimage. 2012;62:2110–2128.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3453527/
Barrett LF, Mesquita B, Ochsner KN, Gross JJ. The experience of emotion. Annual review of psychology. 2007;58:373–373
Corbetta M, Patel G, Shulman GL. The reorienting system of the human brain: From environment to theory of mind. Neuron. 2008;58(3):306–324.
Duncan S, Barrett LF. Affect is a form of cognition: A neurobiological analysis. Cognition and Emotion. 2007;21:1184–1211.
Quattrocki E, Friston K. Autism, oxytocin and interoception. Neurosci. Biobehav. Rev. 2014;47:410–430.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4726659/
Apps M.A., Tsakiris M. The free-energy self: a predictive coding account of self-recognition. Neurosci. Biobehav. Rev. 2014;41:85–97.
Sinha P, et al. Autism as a disorder of prediction. Proc. Natl Acad. Sci. USA. 2014;111:15220–15225.
Paulus MP, Stein MB. Interoception in anxiety and depression. Brain Struct. Funct. 2010;214:451–463.
den Ouden HE, Kok P, de Lange FP. How prediction errors shape perception, attention, and motivation. Front Psychol. 2012 Dec 11;3:548. doi: 10.3389/fpsyg.2012.00548. eCollection 2012.
Fries P: Rhythms for Cognition: Communication through Coherence. Neuron. 2015;88(1):220–35. 10.1016/j.neuron.2015.09.034
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4605134/
Sensory Motor Processing
Butcher PA, Taylor JA. Decomposition of a sensory prediction error signal for visuomotor adaptation. J Exp Psychol Hum Percept Perform. 2018 Feb;44(2):176-194. doi: 10.1037/xhp0000440. Epub 2017 May 15.
Albert ST, Shadmehr R. The Neural Feedback Response to Error As a Teaching Signal for the Motor Learning System. Journal of Neuroscience. 2016;36(17):4832–4845.
Herzfeld DJ, Vaswani PA, Marko M, Shadmehr R. A memory of errors in sensorimotor learning. Science. 2014 1349.
Marko MK, Haith AM, Harran MD, Shadmehr R. Sensitivity to prediction error in reach adaptation. Journal of neurophysiology. 2012;108(6):1752–63.
Izawa J, Pekny SE, Marko MK, Haswell CC, Shadmehr R, Mostofsky SH. Motor learning relies on integrated sensory inputs in ADHD, but over-selectively on proprioception in autism spectrum conditions. Autism Res 5: 124–136, 2012b
Izawa J, Shadmehr R. Learning from Sensory and Reward Prediction Errors during Motor Adaptation. PLoS Comput Biol. 2011;7 e1002012.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3053313/
Schlerf JE, Ivry RB, Diedrichsen J. Encoding of Sensory Prediction Errors in the Human Cerebellum. Journal of Neuroscience. 2012;32(14):4913–4922.
Wei K, Körding K. Relevance of error: what drives motor adaptation? Journal of neurophysiology. 2009;101(2):655–64.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2657056/
Harris-Warrick R.M. Neuromodulation and flexibility in central pattern generator networks. Curr. Opin. Neurobiol. 2011;21:685–692.
De Lazzari F, Bisaglia M, Zordan MA, Sandrelli F. Circadian Rhythm Abnormalities in Parkinson’s Disease from Humans to Flies and Back. Int J Mol Sci. 2018 Dec 6;19(12). pii: E3911. doi: 10.3390/ijms19123911. Review.
Videnovic A., Golombek D. Circadian Dysregulation in Parkinson’s Disease. Neurobiol. Sleep Circadian Rhythm. 2017;2:53–58. doi: 10.1016/j.nbscr.2016.11.001.
Li S., Wang Y., Wang F., Hu L.-F., Liu C.-F. A New Perspective for Parkinson’s Disease: Circadian Rhythm. Neurosci. Bull. 2017;33:62–72. doi: 10.1007/s12264-016-0089-7.
Thaut MH, McIntosh GC, Hoemberg V. Neurobiological foundations of neurologic music therapy: rhythmic entrainment and the motor system. Front Psychol. 2015 Feb 18;5:1185. doi: 10.3389/fpsyg.2014.01185. eCollection 2014. Review.
Auditory Processing
Bizley, Jennifer K, and Yale E Cohen. “The what, where and how of auditory-object perception.” Nature reviews. Neuroscience vol. 14,10 (2013): 693-707. doi:10.1038/nrn3565
Shinn-Cunningham BG. Object-based auditory and visual attention. Trends Cogn Sci. 2008;12:182–186.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699558/
DiCarlo JJ, Zoccolan D, Rust NC. How does the brain solve visual object recognition? Neuron. 2012;73:415–434.
Hill KT, Miller LM. Auditory attentional control and selection during cocktail party listening. Cereb Cortex. 2010;20:583–590.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2820699/
Shamma SA, Elhilali M, Micheyl C. Temporal coherence and attention in auditory scene analysis. Trends Neurosci. 2011;34:114–123.
Middlebrooks JC, Onsan ZA. Stream segregation with high spatial acuity. J Acoust Soc Am. 2012;132:3896–3911.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3528685/
Teki S, et al. Navigating the auditory scene: an expert role for the hippocampus. J Neurosci. 2012;32:12251–12257.
Zonooz B, Van Opstal AJ. Differential Adaptation in Azimuth and Elevation to Acute Monaural Spatial Hearing after Training with Visual Feedback. eNeuro. 2019;6(6):ENEURO.0219-19.2019. Published 2019 Nov 1. doi:10.1523/ENEURO.0219-19.2019
Ahveninen J, et al. Task-modulated “what” and “where” pathways in human auditory cortex. Proc Natl Acad Sci USA. 2006;103:14608–14613.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1600007/
Ding N, Simon JZ. Neural coding of continuous speech in auditory cortex during monaural and dichotic listening. J Neurophysiol. 2012;107:78–89.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3570829/
Shamma S. On the emergence and awareness of auditory objects. PLoS Biol. 2008;6:e155.
Lee AK, Shinn-Cunningham BG. Effects of reverberant spatial cues on attention-dependent object formation. J Assoc Res Otolaryngol. 2008;9:150–160.
Snyder JS, Carter OL, Hannon EE, Alain C. Adaptation reveals multiple levels of representation in auditory stream segregation. J Exp Psychol Hum Percept Perform. 2009;35:1232–1244.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2726626/
King AJ, Nelken I. Unraveling the principles of auditory cortical processing: can we learn from the visual system? Nature Neurosci. 2009;12:698–701.
Obleser J, Leaver AM, Vanmeter J, Rauschecker JP. Segregation of vowels and consonants in human auditory cortex: evidence for distributed hierarchical organization. Front Psychol. 2010;1:232.
Kashino M, Kondo HM. Functional brain networks underlying perceptual switching: auditory streaming and verbal transformations. Phil Trans R Soc B. 2012;367:977–987.
Micheyl C, Kreft H, Shamma S, Oxenham AJ. Temporal coherence versus harmonicity in auditory stream formation. J Acoust Soc Am. 2013;133:EL188–EL194.
Gutschalk A, Micheyl C, Oxenham AJ. Neural correlates of auditory perceptual awareness under informational masking. PLoS Biol. 2008;6:e138.
Micheyl C, et al. The role of auditory cortex in the formation of auditory streams. Hear Res. 2007;229:116–131.
Pressnitzer D, Sayles M, Micheyl C, Winter IM. Perceptual organization of sound begins in the auditory periphery. Curr Biol. 2008;18:1124–1128.
Shamma SA, Micheyl C. Behind the scenes of auditory perception. Curr Opin Neurobiol. 2010;20:361–366.
Riecke L, Micheyl C, Oxenham AJ. Global not local masker features govern the auditory continuity illusion. J Neurosci. 2012;32:4660–4664.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3357484/
Niwa M, Johnson JS, O’Connor KN, Sutter ML. Differences between primary auditory cortex and auditory belt related to encoding and choice for AM sounds. J Neurosci. 2013;33:8378–8395.
Lemus L, Hernandez A, Romo R. Neural codes for perceptual discrimination of acoustic flutter in the primate auditory cortex. Proc Natl Acad Sci USA. 2009;106:9471–9476.
Kilian-Hutten N, Valente G, Vroomen J, Formisano E. Auditory cortex encodes the perceptual interpretation of ambiguous sound. J Neurosci. 2011;31:1715–1720.
Walker KM, Bizley JK, King AJ, Schnupp JW. Multiplexed and robust representations of sound features in auditory cortex. J Neurosci. 2011;31:14565–14576.
Hackett TA. Information flow in the auditory cortical network. Hear Res. 2011;271:133–146.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3022347/
Griffiths TD, Hall DA. Mapping pitch representation in neural ensembles with fMRI. J Neurosci. 2012;32:13343–13347.
Hall DA, Plack CJ. Pitch processing sites in the human auditory brain. Cereb Cortex. 2009;19:576–585.
Griffiths TD, et al. Direct recordings of pitch responses from human auditory cortex. Curr Biol. 2010;20:1128–1132.
Leaver AM, Van Lare J, Zielinski B, Halpern AR, Rauschecker JP. Brain activation during anticipation of sound sequences. J Neurosci. 2009;29:2477–2485.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892726/
Conway C. M., Pisoni D. B., Kronenberger W. G. (2009). The importance of sound for cognitive sequending abilities. Curr. Dir. Psychol. Sci. 18 275–279 10.1111/j.1467-8721.2009.01651.x
Bizley JK, King AJ. Visual–auditory spatial processing in auditory cortical neurons. Brain Research. 2008;1242:24–36.
Moore DR, Hine JE, Jiang ZD, Matsuda H, Parsons CH, King AJ. Conductive hearing loss produces a reversible binaural hearing impairment. J Neurosci. 1999;19(19):8704–8711. doi:10.1523/JNEUROSCI.19-19-08704.1999
Carlile S (2014) The plastic ear and perceptual learning in auditory spatial perception. Front Neurosci 8:237. 10.3389/fnins.2014.00237
Van Wanrooij MM, Van Opstal AJ. Relearning sound localization with a new ear. J Neurosci. 2005;25(22):5413–5424. doi:10.1523/JNEUROSCI.0850-05.2005
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6724994/