Table of Contents
Composition of Whole Blood
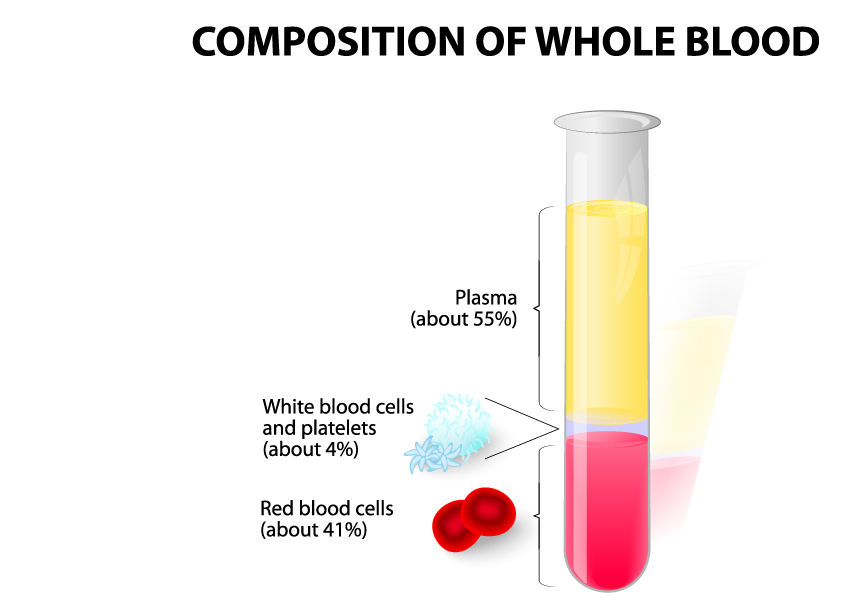
The image illustrates the composition of whole blood as separated by centrifugation. When whole blood is centrifuged, it separates into layers due to the differences in the density of its components.
At the top layer, we have plasma, which constitutes about 55% of whole blood. Plasma is the liquid component of blood, a pale yellow fluid that serves as the medium for carrying blood cells, nutrients, proteins, hormones, and waste products throughout the body.
Below the plasma layer are the white blood cells and platelets, collectively termed the ‘buffy coat.’ Although they make up a relatively small proportion of the blood volume, about 4%, they play crucial roles in the body’s defense mechanisms and blood clotting processes, respectively.
The bottom layer consists of red blood cells, also known as erythrocytes, and they make up about 41% of the blood’s volume. These cells are responsible for transporting oxygen from the lungs to the body’s tissues and carbon dioxide from the tissues back to the lungs.
This image depicts a test tube on the right side, showing the components in their respective proportions after centrifugation, with the plasma at the top, the buffy coat in the middle as a thin layer, and the red blood cells at the bottom. The test tube on the left side shows the components before they are separated, with the whole blood appearing as a uniform liquid.
Blood Composition: Plasma and Its Essential Substances
Blood, the lifeline of our body, is a specialized fluid that comprises several components, each contributing to maintaining our health and facilitating our body’s proper functioning. Among these components, plasma occupies a central role. Accounting for about 55% of the blood’s total composition, plasma is a straw-colored liquid that operates as a transportation highway, carrying a wide array of substances throughout our body.
Plasma’s first crucial role is in nutrient transport. It acts as a carrier, shipping essential nutrients derived from the digestion of food. These nutrients, including glucose, amino acids, fatty acids, vitamins, and minerals, are necessary for the body’s energy production, tissue growth, and overall metabolic processes. Therefore, plasma serves as a crucial link connecting the digestive system with all the body’s cells.
Besides nutrients, plasma also transports hormones, enzymes, and signaling molecules. These substances are integral to chemical communication across different organs and tissues. Hormones, in particular, regulate various bodily functions, ranging from metabolism and growth to reproduction. Enzymes, on the other hand, speed up chemical reactions that are vital for cellular processes. Therefore, plasma plays a significant role in coordinating and regulating body functions through chemical communication.
Oxygen is essential for cell survival and function, and plasma plays a key role in delivering oxygen throughout the body. In the lungs, oxygen binds to hemoglobin in red blood cells, forming oxyhemoglobin. Plasma then carries these oxygen-rich red blood cells to all parts of the body, ensuring efficient oxygen delivery. This process of oxygenation is critical for cellular respiration and energy production.
In addition to delivering essential nutrients and oxygen, plasma is responsible for transporting metabolic waste products. Carbon dioxide, a by-product of cellular respiration, and other waste products are ferried by plasma to organs like the lungs and kidneys, which are responsible for their elimination. This waste transport function ensures that our bodies stay clean internally, maintaining overall metabolic health.
Plasma is also an important part of the immune system, carrying antibodies, complement proteins, and clotting factors. These immune materials play a crucial role in defending the body against infections, healing wounds, and maintaining homeostasis.
Finally, plasma also transports electrolytes (such as sodium, potassium, and calcium), gases (like nitrogen and carbon dioxide), waste materials, and trace elements necessary for various physiological processes. These substances contribute to maintaining the body’s electrolyte balance, gas exchange, and overall health.
In conclusion, blood composition, with its significant plasma component, is a complex mixture of substances that are vital for life. Plasma serves as a multifaceted transport medium, aiding in the delivery of nutrients, facilitating chemical communication, ensuring oxygenation, aiding waste removal, and bolstering immune defenses. Understanding plasma’s roles and the substances it carries can foster a deep appreciation for the incredible capabilities of blood and its indispensable role in health and homeostasis.
Platelets (Thrombocytes)
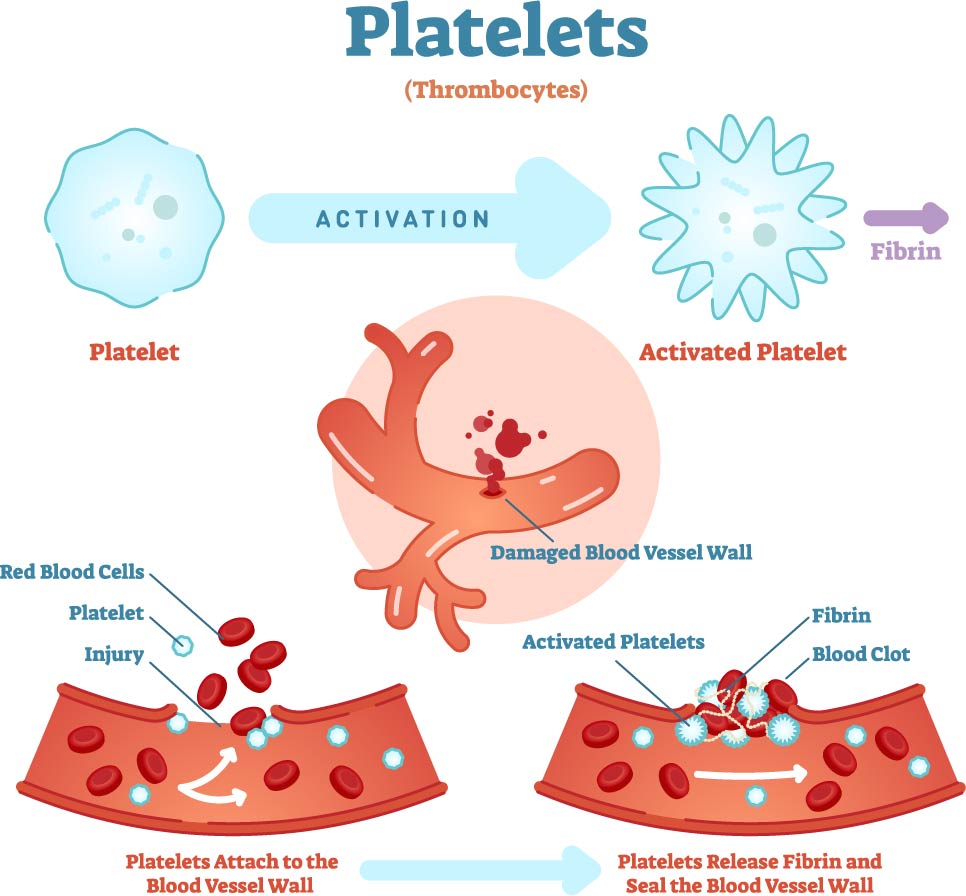
This image provides a visual explanation of the function of platelets, also known as thrombocytes, in the blood clotting process.
At the top, we see two illustrations of a platelet. On the left is a platelet in its inactive state, a small, irregularly shaped cell fragment. On the right, after activation, the platelet changes to a form with extensions, allowing it to interact with other platelets and the damaged vessel wall.
The main section of the image details the steps involved in the formation of a blood clot. Initially, platelets circulate in the bloodstream in their inactive form. Upon encountering a damaged blood vessel, they become activated. This transformation is marked by a change in shape and the expression of surface proteins that allow them to adhere to the vessel wall and to each other.
The first step at the bottom left shows red blood cells and platelets near the site of injury on a blood vessel. The platelets begin to attach to the exposed collagen fibers of the damaged vessel wall.
The second step, at the bottom right, demonstrates how activated platelets release substances that activate other platelets and start the formation of a fibrin mesh. Fibrin is a protein that forms long strands to create a net-like structure. This structure, along with the platelets, forms a stable clot that seals the vessel wall and prevents further blood loss.
Throughout the process, a cascade of biochemical events occurs, which is not depicted here but is crucial for the clot to form and stabilize properly. This sequence is an essential mechanism for preventing excessive bleeding and is the first step in wound healing.
Red Blood Cell Life Cycle
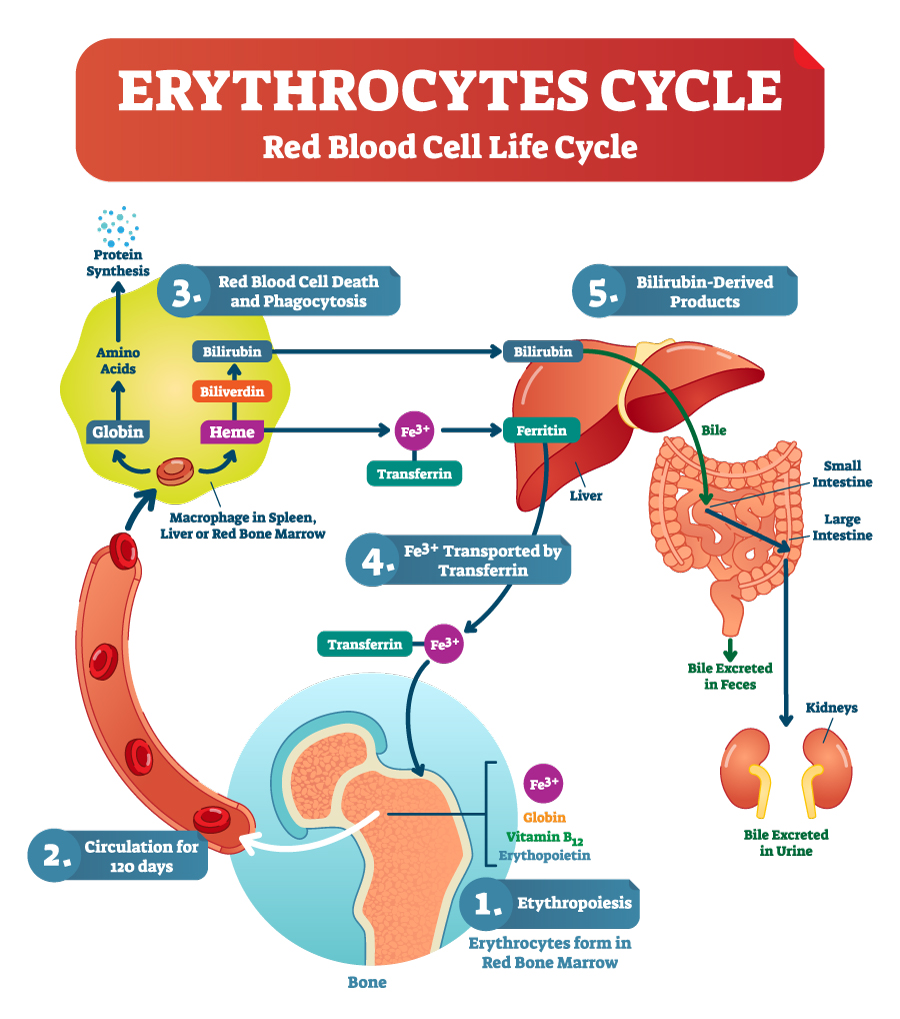
The image details the lifecycle of erythrocytes, or red blood cells, within the human body, highlighting the continuous process from their creation to their breakdown and the recycling of their components.
Erythropoiesis: The cycle begins in the bone marrow, where red blood cells are formed through a process called erythropoiesis. This process is stimulated by the hormone erythropoietin, which is primarily produced in the kidneys in response to low oxygen levels in the blood.
Circulation: Once formed, red blood cells enter the bloodstream and circulate for about 120 days. During their lifespan, they transport oxygen from the lungs to various tissues and carry carbon dioxide back to the lungs for exhalation.
Red Blood Cell Death and Phagocytosis: As red blood cells age, they undergo phagocytosis, primarily in the spleen, but also in the liver and red bone marrow. Macrophages, a type of white blood cell, engulf and break down the old erythrocytes.
Recycling of Components: The breakdown products of red blood cells include globin proteins, which are broken down into amino acids and used in protein synthesis. The heme group from hemoglobin is stripped of its iron (Fe3+) and converted into biliverdin and then to bilirubin. Iron is salvaged and bound to transferrin, a transport protein in the blood, to be transported back to the bone marrow for reuse in new red blood cells.
Bilirubin-Derived Products: Bilirubin is transported to the liver, where it is conjugated and then excreted into the bile. Bile is released into the small intestine and helps with digestion. Bilirubin in the gut is further broken down and eventually excreted from the body in feces, which gives feces its characteristic brown color. A small amount is also excreted through the kidneys into the urine.
The process efficiently recycles valuable components, like iron, while eliminating waste products, demonstrating the body’s ability to maintain homeostasis and resource conservation.
Hematopoiesis: Blood Cell Formation
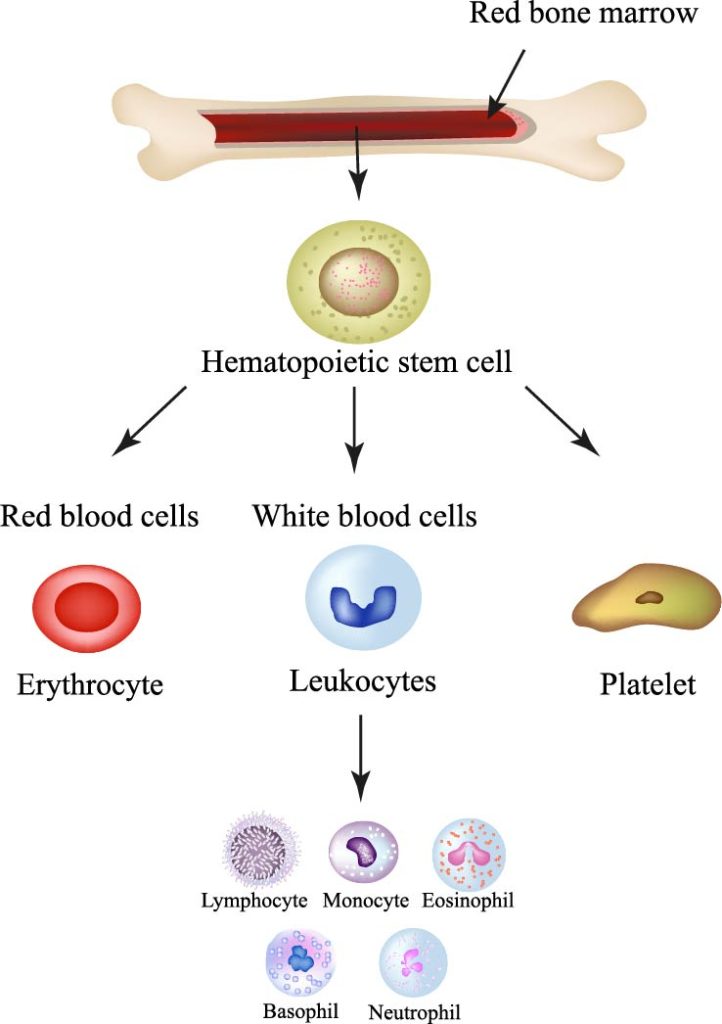
The image provides a simplified view of hematopoiesis, the process of blood cell formation, which occurs in the red bone marrow.
At the top, the red bone marrow is depicted within a bone, highlighting its role as the primary site for hematopoiesis. The bone marrow contains hematopoietic stem cells, which are multipotent stem cells with the ability to give rise to all the different blood cells required by the body.
These hematopoietic stem cells differentiate into three main types of blood cells:
Red blood cells (erythrocytes): These cells are represented by a simple red disc, reflecting their biconcave shape, which increases their surface area for oxygen exchange. Erythrocytes are responsible for transporting oxygen from the lungs to the body’s tissues and returning carbon dioxide to the lungs for exhalation.
White blood cells (leukocytes): Illustrated as a blue, lobed structure, these cells are part of the immune system and protect the body against both infectious disease and foreign invaders. The image further breaks down leukocytes into five subtypes:
- Lymphocytes, which are involved in the adaptive immune response. There are two main types, B-cells that produce antibodies and T-cells that attack infected cells.
- Monocytes, which develop into macrophages and dendritic cells that are crucial for phagocytosis (engulfing and digesting cellular debris and pathogens) and antigen presentation, respectively.
- Eosinophils, which are involved in combating multicellular parasites and also play a role in allergic reactions.
- Basophils, which release histamine and play a role in inflammatory responses, particularly allergic reactions.
- Neutrophils, which are the most numerous of the white blood cells and form the first line of defense against pathogens.
Platelets (thrombocytes): Shown as a small, irregularly shaped cell fragment, platelets are crucial for blood clotting. They aggregate at sites of vascular injury, adhering to the vessel wall and each other to form a hemostatic plug that minimizes blood loss.
This image serves as an educational tool to understand the origin of blood cells and their primary functions in the body’s circulatory and immune systems.
Platelet Clotting Process
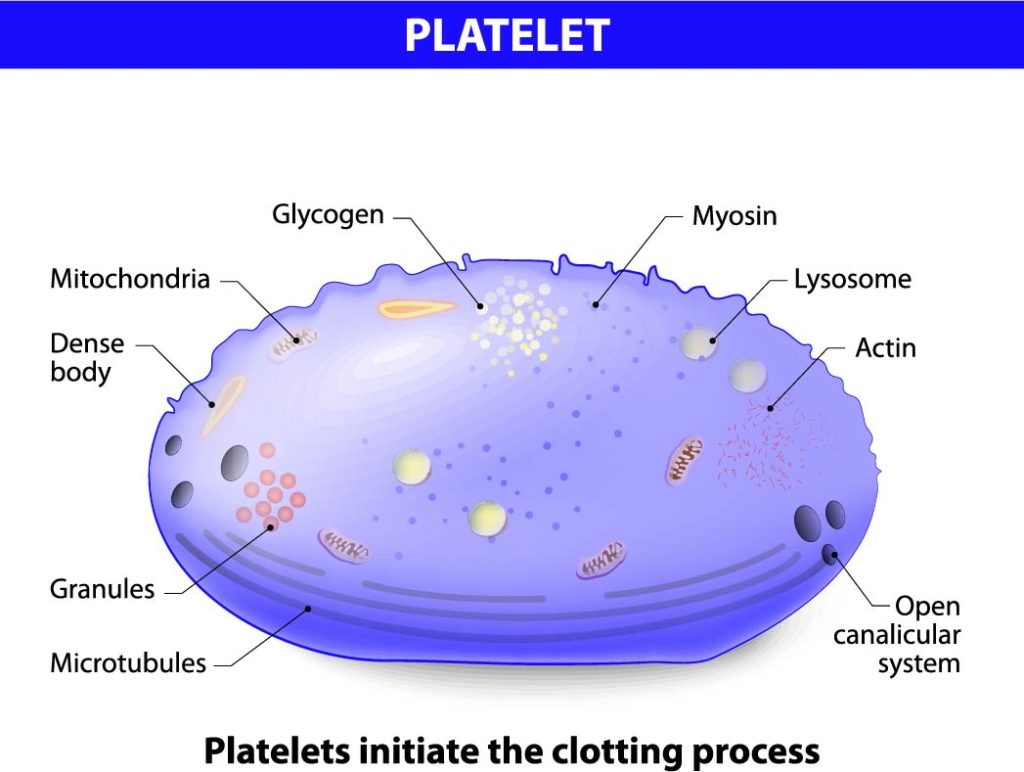
The image provides a detailed representation of the internal structure of a platelet, which plays an essential role in hemostasis, the process that stops bleeding at the site of an injury.
A platelet is shown with several key components labeled:
- Mitochondria are present in the platelet, providing energy in the form of ATP necessary for the platelet’s activation and aggregation during the clotting process.
- Dense bodies are small granules that contain non-metabolic pools of calcium, ADP, ATP, and serotonin, which are secreted upon platelet activation to promote aggregation and vasoconstriction.
- Granules are storage sites for a variety of substances crucial to platelet function, including growth factors, clotting factors, and other molecules that regulate the clotting process and wound healing.
- Microtubules, depicted as circular structures within the platelet, maintain the platelet’s discoid shape and play a role in the release of granule contents during activation.
- Glycogen is a storage form of glucose, which serves as an energy reserve that can be mobilized when needed.
- Myosin, along with actin (not labeled but implied), forms part of the cytoskeleton and is involved in the contractile events that lead to the change in platelet shape during activation and the formation of a platelet plug.
- Lysosomes contain digestive enzymes that can break down ingested materials or damaged cellular components.
- Actin filaments are part of the cytoskeleton, which helps in maintaining the platelet’s shape and is involved in the contraction and expansion during the clotting process.
- The open canalicular system is a system of membrane-bound channels within the platelet that serves as a pathway for the transport of substances in and out of the platelet.
At the bottom of the image, it is emphasized that “Platelets initiate the clotting process.” When there is vascular damage, platelets adhere to the exposed collagen fibers, become activated, change shape, and release the contents of their granules to recruit more platelets and form a platelet plug. This plug temporarily seals small breaks in the blood vessel wall, and the substances released from the granules further promote blood clotting by activating additional clotting factors.
Neutrophil Anatomy
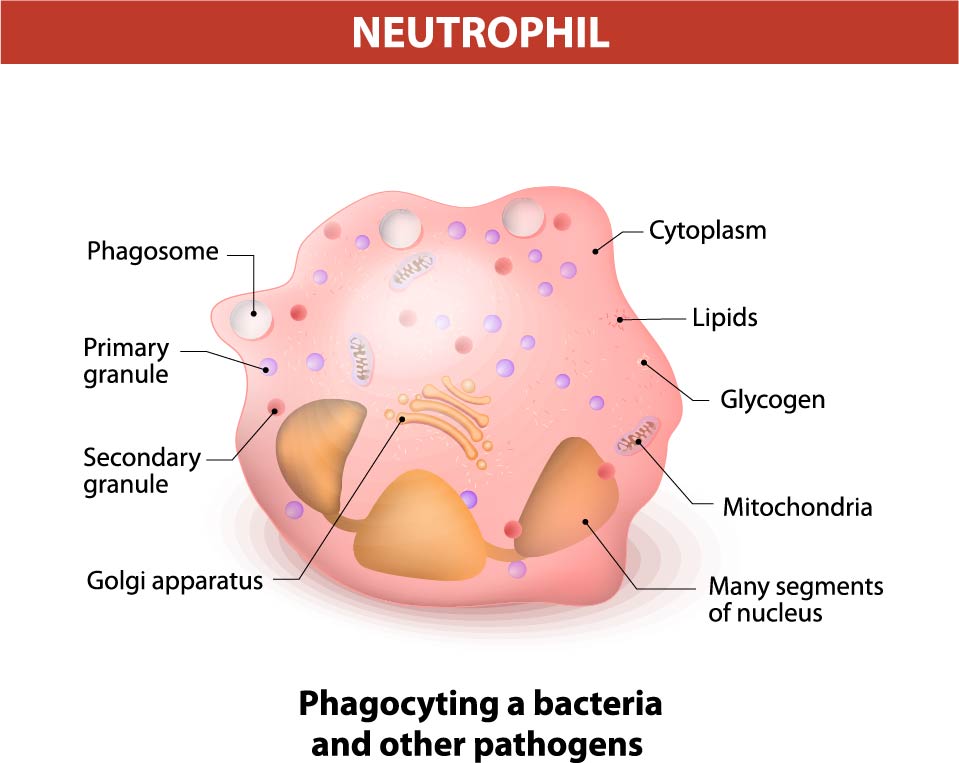
The image illustrates a neutrophil, which is a type of white blood cell that is a key component of the innate immune system. Neutrophils are primarily involved in the defense against infections, especially bacterial infections, through a process called phagocytosis.
Highlighted features of the neutrophil include:
- Cytoplasm: This jelly-like substance fills the cell, providing a medium for the organelles to be suspended and held in place within the cell.
- Lipids: These organic compounds are part of the cell membrane and also serve as an energy reserve.
- Glycogen: Similar to lipids, glycogen is a stored form of energy that the cell can use when needed.
- Mitochondria: Known as the powerhouses of the cell, these organelles generate the energy currency of the cell, ATP, through respiration and to regulate cellular metabolism.
- Many segments of the nucleus: Neutrophils are characterized by their multi-lobed nucleus, usually with 3-5 lobes, which is a distinguishing feature when viewed under a microscope.
- Golgi apparatus: An organelle involved in the modification, sorting, and packaging of proteins for secretion. It is also involved in the formation of granules.
- Primary granule: These granules, also known as azurophilic granules, contain enzymes and proteins that are used to digest microorganisms engulfed by the neutrophil.
- Secondary granule: Also known as specific granules, these contain a different set of enzymes that are also antibacterial in function but are more specific than those in the primary granules.
- Phagosome: A vesicle formed around a particle engulfed by phagocytosis. It is an essential part of the neutrophil’s mechanism to ingest and break down pathogens.
The bottom of the image states “Phagocytosing a bacteria and other pathogens,” which is the primary function of neutrophils. During phagocytosis, neutrophils engulf pathogens into phagosomes, which then fuse with granules to form a phagolysosome where the pathogen is destroyed. Neutrophils are among the first cells to arrive at the site of infection, and their activity is critical in the early stages of the inflammatory response to infection.
Music Library
Platelets: Rhythm of the Clots
[Verse] In the body, there’s a rhythm so fine A dance of cells, workin’ overtime Platelets be their name, they’re in the fight Clumpin’ together, creatin’ clots so tight
[Verse 2] Irregular-shaped, like little pieces of art Activated at injury sites, they start They bind and form a plug, stop the bleed Essential for the body, a critical need
[Chorus] Platelets, oh platelets, keepin’ us alive Clotting the blood, helpin’ us thrive Oh platelets, oh platelets, we thank you so For your dance in our veins, we’re all aglow (ooh-yeah)
Neutrophils: Battle Cry
[Verse] Infiltrate the chaos, the battle’s just begun A solitary soldier fighting underneath the sun Racing through the bloodstream, with a purpose and a plan
Neutrophil’s the name, protector of the land (Phagocytosis, oh yeah) Engulf and neutralize, the enemy’s demise (Phagocytosis, oh-oh-oh) With every beat of my cell, infection’s bound to quell
[Chorus] I’m a warrior inside, ready to take on the fight Phagocytosis, my battle cry tonight I’ll defend against the invaders, the bacteria they send Neutrophil’s on guard, no mercy to extend
Fluids and the Circulatory System
Fluids are the lifeblood of our bodies, performing a multitude of essential functions. Among these fluids, blood stands out due to its vital roles in carrying nutrients and oxygen to cells, and removing waste products. However, the journey of blood and the circulation of fluids in the body is a complex process that involves several systems, including the cardiovascular and lymphatic systems. To gain a deeper understanding of these processes, let’s delve into the composition of blood, how it circulates, and the role of interstitial fluid.
The journey of plasma, the fluid part of blood, begins as it moves through the capillary walls. Here, it becomes the interstitial fluid in the extracellular matrix, the space outside our cardiovascular vessels. This extracellular matrix, also referred to as the interstitial space, is the place where fluids interact with cell surfaces. They deliver nutrients, oxygen, and other essential resources, playing a crucial role in ensuring proper cellular operation. Comprising water, oxygen, ions, beneficial chemicals like hormones, and immune materials, interstitial fluid is present in all tissues of our body.
The immune system, in its role as the body’s defender, breaks down large molecules and foreign substances, processing them within the lymphatic system. Occasionally, toxic and foreign substances may not be immediately processed, remaining quarantined in tissues indefinitely.
When it comes to circulation, our heart is the main engine, pumping blood through arteries that distribute it throughout the body. These arteries branch into different areas, including the head, abdomen, and extremities. They continue branching until they reach the cellular level, becoming capillaries. The blood flows through a series of valves based on the immediate needs of the cells. Plasma, the fluid part of blood, is forced out of capillaries, providing nourishment and resources to cells while red blood cells remain within the bloodstream.
As plasma is pushed out of capillaries into the extracellular space, it becomes interstitial fluid. This fluid slowly passes through the proteoglycan gel and across cell surfaces, providing nourishment and supplies to cells. Fluid not utilized by cells is then removed by veins or lymphatic vessels. Negative fluid pressure creates suction into lymphatic capillaries. Interestingly, the inlet valves of these capillaries are connected to surrounding fascial fibers, enabling them to open wider when fluid volume and pressure increase, thus preventing edema.
Unlike the cardiovascular system, the lymphatic system doesn’t have an internal pump like the heart. Instead, it relies on muscle movement to propel fluid flow, which consequently reduces during periods of inactivity. Lymphatic vessels are equipped with valves designed to prevent fluid from moving backward due to gravity.
Lymph nodes play a crucial role in the lymphatic system. These nodes consist of a series of sinuses where fluid is cleansed along the return route to the heart. Sinuses can become clogged if there is a restriction in fluid flow or if the nodes are overwhelmed with toxins. They clean fluids by breaking down toxins into smaller particles for processing. The largest clusters of lymph nodes are found in various locations, including behind the knees, at groin leg creases, armpits, face, neck, upper chest, and deep inside the abdomen. Finally, the lymphatic system empties into the Subclavian Vein behind the left collarbone.
In conclusion, understanding the composition of blood, the circulation of fluids through the cardiovascular and lymphatic systems, and the role of interstitial fluid is essential for comprehending the body’s intricate mechanisms. Familiarizing yourself with these processes will provide insights into how fluids nourish cells, the importance of lymphatic flow, and the vital role of blood in sustaining overall health.
Anatomical Terms and Definitions
| Term | Definition |
|---|---|
| ATP | Adenosine triphosphate, a molecule that carries energy within cells for metabolism. Present in platelets, it's necessary for activation and aggregation during the clotting process. |
| Buffy Coat | A thin layer in centrifuged blood that contains white blood cells and platelets, crucial for body's defense mechanisms and blood clotting processes, respectively. |
| Dense Bodies | Granules within platelets that contain substances like calcium and serotonin, essential for clotting and vasoconstriction upon platelet activation. |
| Erythropoiesis | The process of red blood cell formation in the bone marrow, stimulated by erythropoietin in response to low oxygen levels. |
| Erythropoietin | A hormone primarily produced by the kidneys that stimulates the production of red blood cells in the bone marrow. |
| Fibrin | A protein involved in blood clotting, forming a mesh that traps platelets and cells to create a clot. |
| Granules | Structures within platelets and neutrophils containing various substances crucial for their function in clotting and immune response, respectively. |
| Hematopoiesis | The process of blood cell formation, occurring in the red bone marrow and giving rise to red blood cells, white blood cells, and platelets. |
| Hemoglobin | A protein in red blood cells responsible for carrying oxygen from the lungs to the body's tissues and returning carbon dioxide to the lungs. |
| Hemostasis | The process that stops bleeding at the site of an injury, involving the activation, aggregation, and adhesion of platelets to form a clot. |
| Lysosomes | Organelles containing digestive enzymes, present in platelets for breaking down ingested materials or damaged cellular components. |
| Microtubules | Structural components within platelets that maintain their shape and are involved in granule release during activation. |
| Mitochondria | Organelles that produce energy (ATP) for cell functions, found in platelets for clotting process activation and in neutrophils for defending against infections. |
| Neutrophil | A type of white blood cell that is part of the innate immune system, involved in defending the body against infections through phagocytosis. |
| Phagocytosis | The process by which cells, like neutrophils and macrophages, engulf and digest pathogens or debris. |
| Plasma | The liquid component of blood, making up about 55% of its volume, that carries blood cells, nutrients, proteins, hormones, and waste products. |
| Platelets (Thrombocytes) | Small, irregularly shaped cell fragments in the blood, crucial for clotting. They activate and aggregate at injury sites, initiating the clotting process. |
| Red Blood Cells | Also known as erythrocytes, these cells transport oxygen from the lungs to the body's tissues and carbon dioxide back to the lungs. They make up about 41% of blood’s volume. |
| White Blood Cells | Part of the immune system, these cells protect the body against both infectious disease and foreign invaders. They are depicted in the hematopoiesis process as differentiating into various types, including lymphocytes, monocytes, eosinophils, basophils, and neutrophils. |

